Has Tuberculosis Contributed to the Global Rates of Cystic Fibrosis?
Cystic Fibrosis is not a disease new to modern history. It is speculated that people have died from the disease for hundreds if not thousands of years. If cystic fibrosis, which is terminal in the majority of patients, is in fact thousands of years old, how then has it persisted and even thrived for hundreds of generations rather than subsiding out over time?
Several studies, spurred by this question, have speculated that cystic fibrosis has continued to persist through a selective advantage conferred to CF carriers, thereby increasing the probability that the carrier will live to pass on the CF mutation to following generations.
What then is the difference between a carrier and someone who has cystic fibrosis? Each person contains two of every gene, one provided from the mother and the other from the father. Cystic fibrosis results when both copies of the CFTR gene are mutated. Therefore, a carrier is someone who does not have the disease but contains a mutation in one of his or her CFTR genes but their second CFTR gene is normal. A person then is only born with CF if they receive two mutated CFTR genes, one from their mother and one from their father, both of whom would be CF carriers.
Scientists have hypothesized that carriers of cystic fibrosis possess a selective advantage better protecting them against the illnesses typhoid and tuberculosis caused by bacterial infection. The idea is that if a person is better able to survive these illnesses because of their mutated CFTR gene then they will have an increased likelihood of passing their mutated gene onto following generations. In this way, CFTR mutations responsible for cystic fibrosis could continue to be passed down through time.
Ask questions and share your knowledge of Cystic Fibrosis in our forums.
This, however, raises the obvious question of how is it possible that a CF mutation, which is often considered harmful, is able to provide protection from typhoid and tuberculosis? The answer to this is found in how the bacteria interact with the CFTR chloride channel during infection.
Salmonella typhi is the bacterium responsible for typhoid fever, and has been found to enter intestinal cells during infection through attachment to the CFTR channel. The CFTR channel serves almost as a door or gate, allowing bacteria into cells to begin infection. Since CF carriers posses a reduced number of CFTR channels, it reduces the number of ways that the bacteria has to enter the cell and decreases the likelihood of infection.
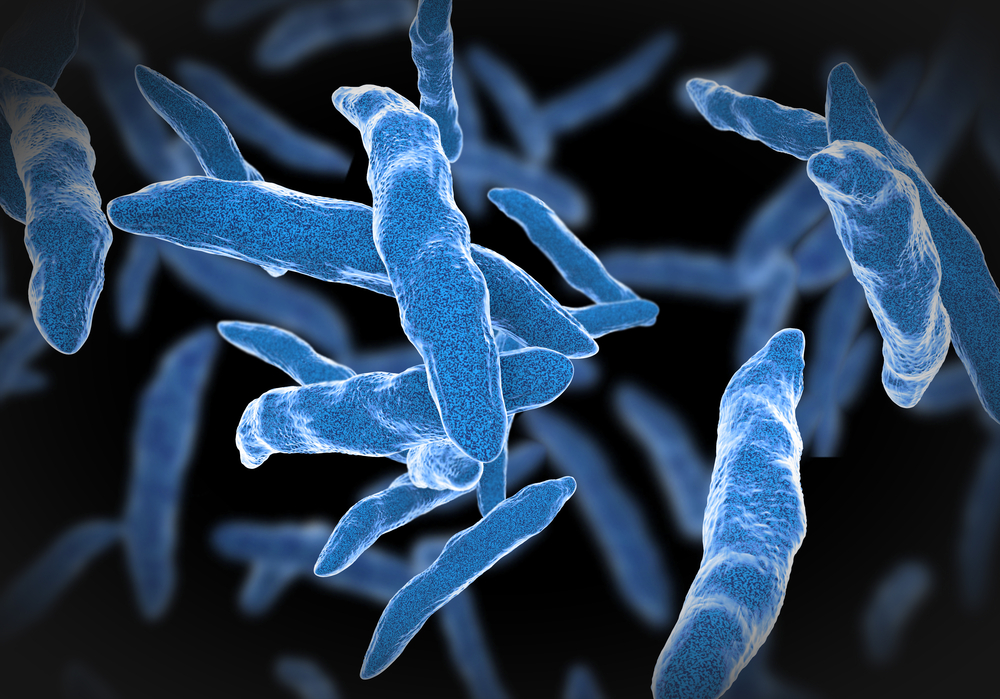
By a slightly different mechanism, CF carriers are also protected against tuberculosis through an indirect interaction within the cell. Mycobacterium tuberculosis, the bacterium for tuberculosis, incorporates sulfate into its cell walls. CF carriers, however, have a reduced activity of arylsulfatase B activity, which is used by the bacteria to incorporate sulfate. The inability of M. tuberculosis to utilize sulfate in the synthesis of its cell walls reduces its virulence and provides protection to the CF carrier.
Although mutations in the CFTR gene provide protection against both typhoid and tuberculosis it has been proposed that tuberculosis alone is the selective agent that provides the best explanation for the global incidence of CF with the highest rates for the disease found in caucasion populations descended from Europe with rates ranging from 1 in 2,000 to 3,500 live births.
One study titled “Evaluating Candidate Agents of Selective Pressure for Cystic Fibrosis” used predictive models to determine the contribution of cholera, typhoid and tuberculosis to the current, global incidence of cystic fibrosis and determined that only tuberculosis, due to its severe outbreak in Europe in the seventeenth century could account for the modern incidence of CF in populations descended from those European countries.
“The tuberculosis pandemic, the ‘white plague’ that claimed over 20% of all European lives beginning in the 1600s, swept across the world over subsequent centuries. However, its origin and duration in Europe meant that the greatest selective pressure was applied there — enough so that, according to our results, tuberculosis resistance in the CF heterozygote can explain the modern gradient in CF incidence between Europe and the rest of the world.”
The study goes on to predict that, “in situations where tuberculosis is no longer responsible for significant mortality among individuals of reproductive age, our model demonstrates that the incidence of CF will fall. The decline amounts to a 0.1% decrease in CF incidence annually over the next 100 years. To reduce the incidence by half requires approximately 20 generations.”
Although the study is only a prediction for the role of tuberculosis in increasing the rates of CF it provides an interesting explanation for the current, global distribution of the disease. Fortunately, with the modern developments in personalized medicine, and genome editing techniques such as CRISPR, we may not have to wait 20 generations for a dramatic decline in the rates of CF.