Antibiotic Combination Kills Resistant Bacteria Affecting CF Patients, Study Reports
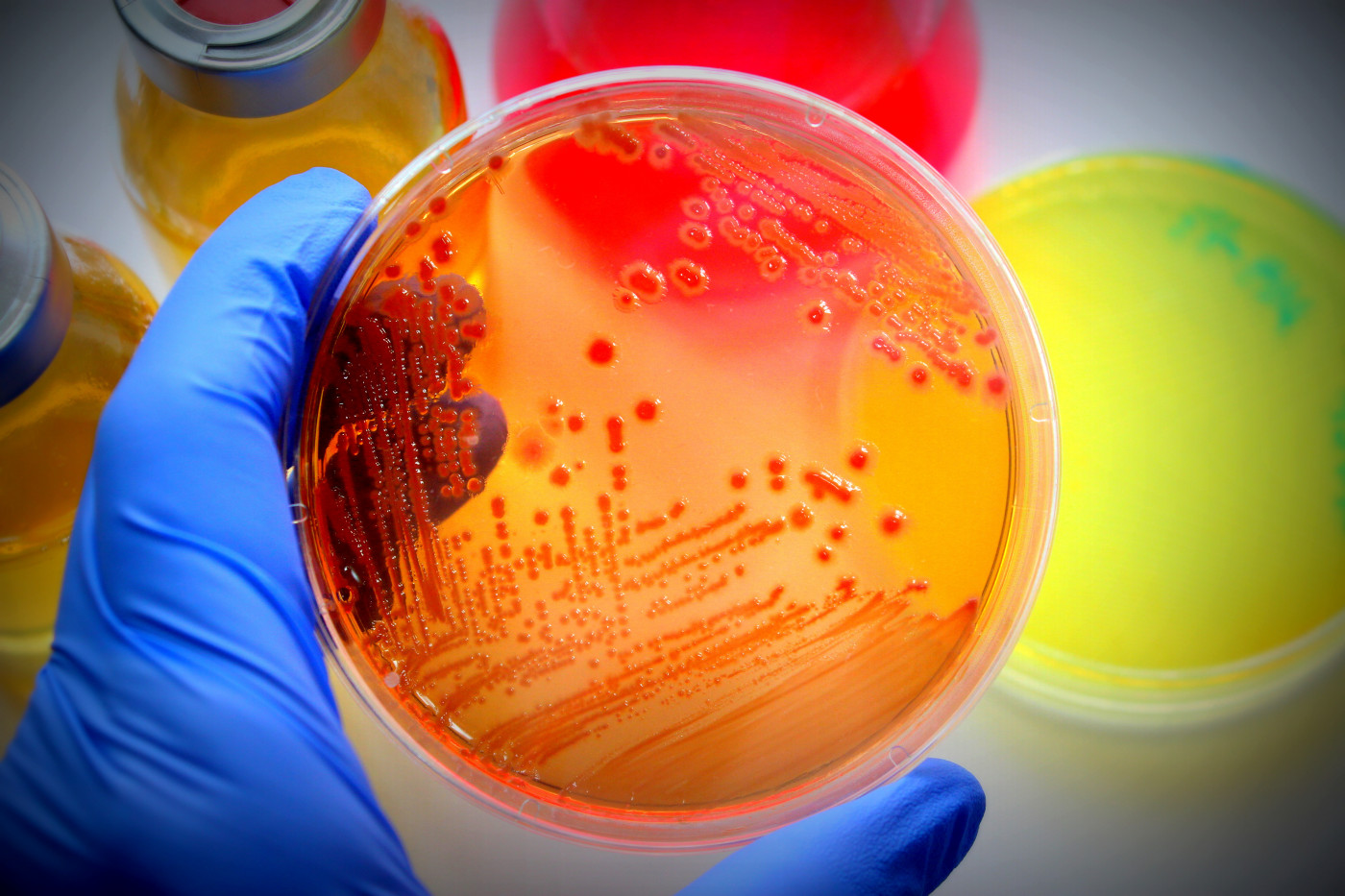
A triple-antibiotic combination completely eliminated antibiotic-resistant Mycobacterium abscessus, a bacterial infection especially dangerous to people with cystic fibrosis (CF), a study found.
Combined doses of three antibiotics — amoxicillin, imipenem, and relebactam — were effective at killing M. abscessus isolated from CF patients.
The study, “Effect of Amoxicillin in combination with Imipenem-Relebactam against Mycobacterium abscessus,” was published in the journal Nature Scientific Reports.
People with CF are susceptible to opportunistic infections, including one caused by a non-tuberculous mycobacteria (NTM) called Mycobacterium abscessus.
M. abscessus infection is resistant to many so-called beta-lactam antibiotics, including penicillin and amoxicillin, because it has an enzyme — beta-lactamase — that breaks down the antibiotics before they can act.
Medicines have been developed to selectively inhibit the beta-lactamase enzyme, and some have been used in combination to prevent their breakdown.
People with M. abscessus infection often are treated with imipenem (marketed as Primaxin by Merck), which has the highest activity against M. abscessus and cannot be broken down by the beta-lactamase enzyme.
The combination of relebactam (a beta-lactamase inhibitor), imipenem and cilastatin (a compound that blocks the metabolism of relebactam) — together known as Recarbrio and marketed by Merck — was approved by the U.S. Food and Drug Administration in 2019 to treat urinary tract and abdominal bacterial infections. (Notably, Merck is known as MSD outside of the U.S. and Canada.)
Researchers at Aston University in the U.K. tested both imipenem and relebactam, together with amoxicillin, against bacterial samples (isolates) taken from 16 infected CF patients.
In all cases, the addition of relebactam made the bacteria fully susceptible to the action of amoxicillin, resulting in 100% elimination of M. abscessus bacteria.
As expected, imipenem alone was effective against M. abscessus; however, its effectiveness was enhanced by the addition of relebactam, and improved even more with the addition of amoxicillin.
With the addition of amoxicillin, four times less imipenem and relebactam were needed to achieve the same inhibitory effect.
A triple-combination therapy that is effective at lower doses may lessen the side effects of established treatments, improving the health, quality of life, and survival chances of infected CF patients.
“Our findings represent a timely and highly impactful discovery that could be easily translatable into the clinical setting, providing a new therapeutic option for M. abscessus infections,” the researchers said.
“Our new drug combination is significantly less toxic than those currently used, and so far we have managed to kill every patient’s bacterial isolate that we have received,” Jonathan Cox, PhD, a lecturer in microbiology at Aston University and the team’s leader, said in a press release.
“Because amoxicillin is already widely available, and imipenem-relebactam has just been approved for use by the Food and Drug Administration in the U.S., these drugs are already available to clinicians,” Cox said. “We therefore hope to start treating patients as soon as possible.”
The next step will be to test the combination on infected CF patients, and compare it to antibiotics already available.
“Mycobacterium abscessus, also known as NTM, is the most feared infection a person with cystic fibrosis can develop,” said Paula Sommer, PhD, head of research at the Cystic Fibrosis Trust in the U.K. “Taking drugs to treat NTM can add to an already significant regime of daily treatments, and take up to a year to clear infections. We look forward to a time when effective, short courses of treatment are available to treat NTM.”