Common Lung Infections Can Be Identified by Collecting Sputum and Throat Swabs, Study Shows
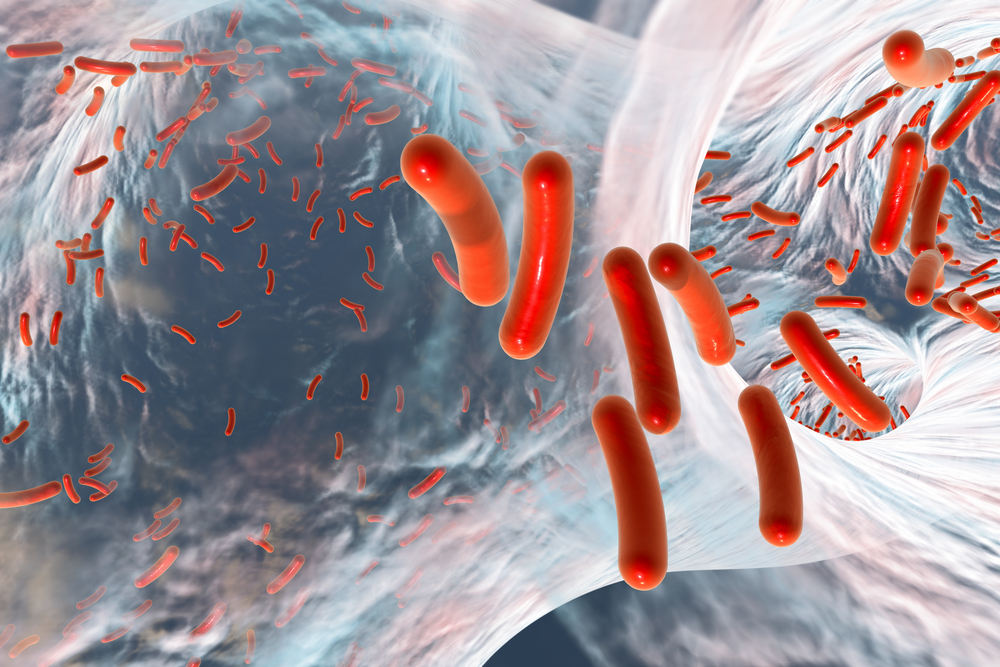
A recent study has shown that sputum and throat swabs of adult cystic fibrosis (CF) patients can be used to identify Pseudomonas aeruginosa and Staphylococcus aureus lung infections.
CF patients frequently suffer from chronic respiratory infections and inflammation, which ultimately can lead to respiratory failure, the major cause of morbidity and mortality in CF. An accurate assessment of which microorganisms are responsible for the CF patients’ lung infections is critical to allow a more suitable therapy.
In the study “Throat Swabs and Sputum Culture as Predictors of P. aeruginosa or S. aureus Lung Colonization in Adult Cystic Fibrosis Patients,” published in the scientific journal Plos One, researchers aimed to determine whether collection of throat swabs or sputum could be used as reliable methods to identify common microorganisms infections in adult CF patients.
Twenty adult CF patients underwent bronchoalveolar lavage (BAL), a diagnostic procedure in which a washing liquid is introduced in the lungs and recollected to allow identification of pulmonary infections. CF patients also provided sputum samples when they could spontaneously expectorate. Throat swabs were also collected from all patients.
The samples were analyzed by standard microbiology testing to determine the presence of P. aeruginosa and S. aureus, which are according to the Cystic Fibrosis Foundation, the two most common microorganisms infecting CF patients.
Researchers compared the results obtained by the BAL analysis with the ones obtained through the sputum and the throat swab testing.
P. aeruginosa infection was detected in both sputum and throat swabs with an efficiency of 100% compared to BAL results. However, these methods were not able to predict as accurately the negative cases of P. aeruginosa infection. Indeed, they could correctly predict only 60% (by sputum testing) and 50% (by throat swab testing) of the P. aeruginosa non-infected patients.
For the detection of S. aureus infection, these two methods were not as sensitive. Sputum analysis could positively detect only 57% of the CF-infected patients, and the throat swab analysis could positively detect only 41%. Nevertheless, these methods correctly identified all the S. aureus non-infected CF patients.
“Our data show that positive sputum and throat culture findings of P. aeruginosa reflect results found on BAL fluid analysis, suggesting these are reasonable surrogates to determine lung colonization with P. aeruginosa,” the researchers concluded in their article. “However, sputum and throat culture findings of S. aureus do not appear to reflect S. aureus colonization of the lung,” they said.
The authors suggest that further studies are needed to determine the accuracy of throat and sputum analysis in representing lung-associated microorganisms. In addition, these results need to be confirmed in a larger and more diverse CF patient population.