Stem Cell Transplant Into Airways Might Treat CF, Mouse Study Suggests
A study in mice showed it is possible to transplant stem cells into the lungs and replenish the airways with healthy cells, an approach that could combat cystic fibrosis and alleviate its symptoms.
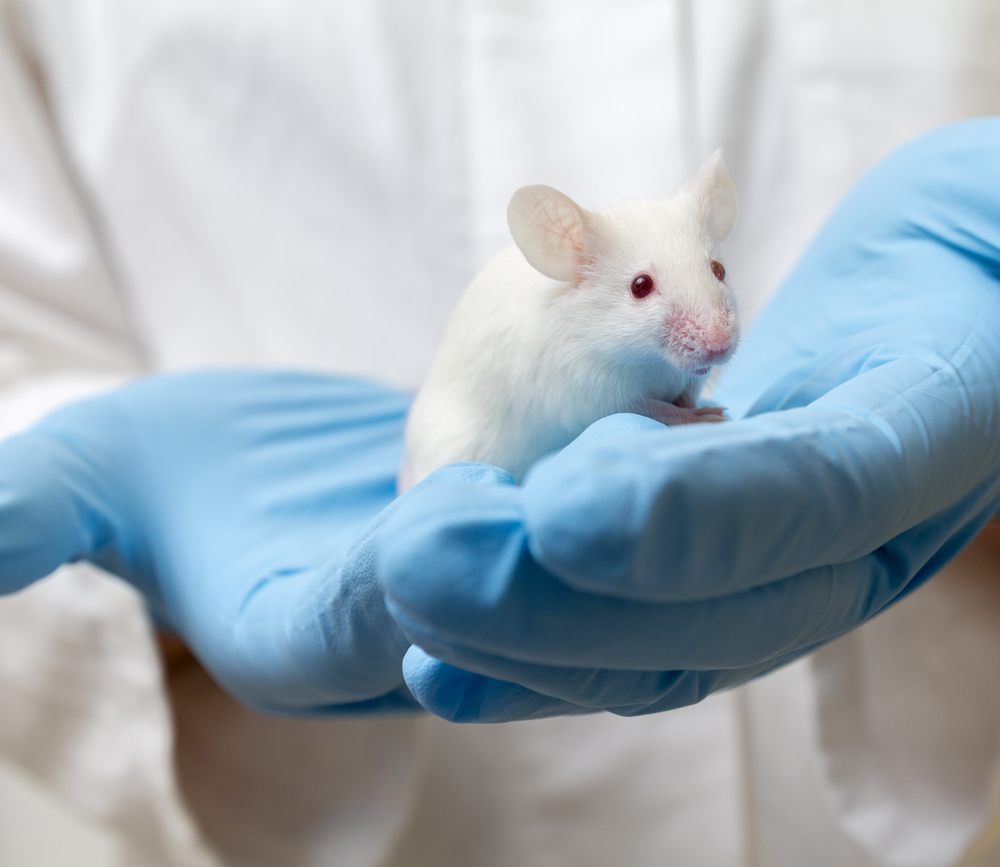
Researchers used stem cells from the airways of cystic fibrosis (CF) patients, which were corrected to produce a normal CFTR gene before being implanted in mice.
The study, “Epithelial disruption: a new paradigm enabling human airway stem cell transplantation,” was published in the journal Stem Cell Research & Therapy.
Cell transplant therapy has been applied successfully in patients with blood and immunodeficiency disorders, in which patients receive stem cells that carry the capacity to regenerate their immune system.
With this in mind, researchers aimed to develop a similar strategy for CF where patients would receive their own stem cells, previously corrected for the CFTR gene – the underlying cause of CF – with gene therapy.
“Our research which applies stem cell transplantation, involves harvesting adult stem cells from the lungs of CF patients, correcting them with gene therapy, and then reintroducing those cells back into the patient,” Nigel Farrow, PhD, a post-doctoral research fellow at the University of Adelaide’s Robinson Research Institute and study first author, said in a press release.
“The new transplanted adult stem cells pass on their healthy genes to their ‘daughter cells’ providing a constant means to replenish the airways with healthy cells, and thereby combating the onset of cystic fibrosis airway disease,” he added.
Researchers used two kinds of stem cells that could differentiate into the myriad cells in the airways. One was obtained from the airways of CF patients; the other came from the placenta, which may represent cells from donors. Both cell types had a gene for bioluminescence, which enabled researchers to follow their location and determine the success of the transplant.
To improve the effectiveness of the transplant, researchers took a novel approach. Prior to receiving the cells, mice were treated with a chemical — polidocanol (PDOC) — that disrupted their epithelial lung barriers. (Epithelium is the layer of cells that covers the entire airways.)
The approach aimed to eliminate these cells, so that the transplanted cells would have space to attach and grow.
“The key to these successful transplantations was our innovative method; we first eliminated the existing surface cells, which then created the space required to introduce the new cells,” said Farrow.
Some received the transplant two hours after the PDOC treatment and others received it 24 hours after treatment. A third group, used as controls, received a saline solution instead of PDOC.
Results showed that only mice that received the transplant two hours after PDOC treatment had signs of stem cells at one and three weeks after the therapy. Mice receiving a saline solution of the transplant 24 hours after PDOC did not have any stem cells in their airways.
In mice where the transplant was successful, researchers saw a decrease in stem cells after five weeks, which reached similar levels as controls by week eight.
Overall, “this study shows that human airway basal stem cells can be transplanted into live (mouse) airway if the epithelium is first denuded or damaged,” researchers wrote.
While the study is preliminary and further optimization is required, these findings suggest the potential for human airway stem cells transplantation as a therapy for CF and other lung diseases.
“If we can perfect this technique, it will accelerate this exciting research which could significantly improve the lives of those living with cystic fibrosis and potentially combat this chronic life-limiting illness,” said Farrow.