Immunotherapy May Be Promising Strategy to Treat Chronic Infections of P. aeruginosa in CF Patients
Blocking the interaction between two molecules involved in immune restraining mechanisms — called PD-1 and PD-L1 — may be an effective therapeutic strategy to boost the immune system and treat chronic infections of Pseudomonas aeruginosa in cystic fibrosis (CF) patients, according to a recent study.
The study, “Pseudomonas aeruginosa colonization causes PD-L1 overexpression on monocytes, impairing the adaptive immune response in patients with cystic fibrosis,” was published in the Journal of Cystic Fibrosis.
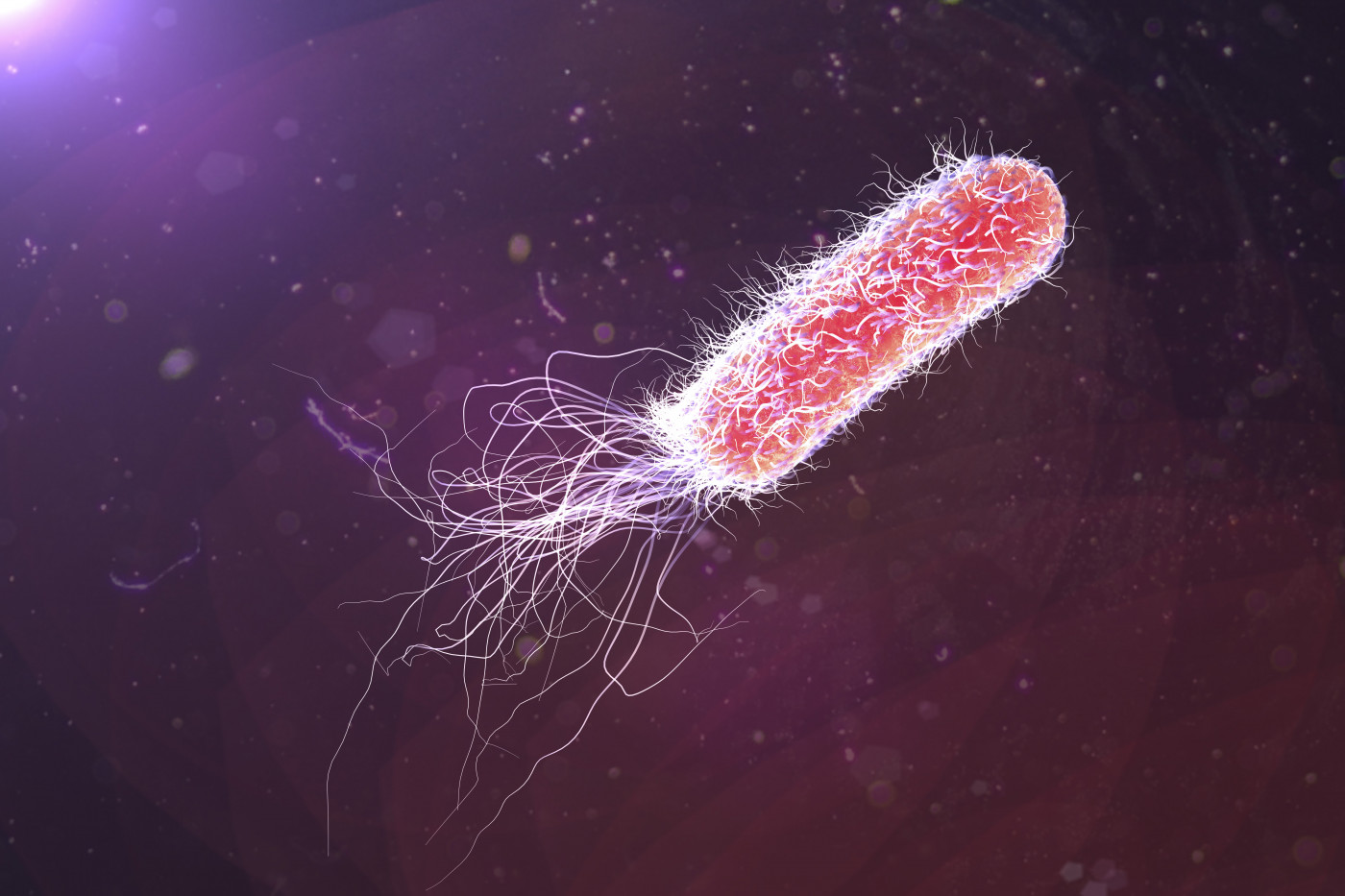
Chronic lung infections by P. aeruginosa — a highly antibiotic-resistant bacteria — are the leading cause of death among CF patients.
The high frequency of infections in CF patients suggest they have an impaired immune system. Furthermore, previous studies have shown that these patients have what is called an endotoxin tolerance, meaning a reduced responsiveness to pathogens following a first contact, leading to a desensitization of immune cells against them.
Join the Cystic Fibrosis News Today forums: an online community especially for patients with CF.
Researchers have proposed that the passage of bacteria to the bloodstream, inducing a systemic exposure to their LPS — a major component of the cell wall of some bacteria, including P. aeruginosa, that is recognized by the body’s immune system as foreign —, either attached to the membrane or in a soluble form, may explain the endotoxin tolerance observed in CF patients.
Recent evidence has shown that PD-L1 is a marker of endotoxin tolerance. PD-L1/PD-1 interaction has emerged as an important mechanism in the immune response, where the binding of PD-L1, present in many cells, to its PD-1 receptor on immune T-cells prevents the activation of T-cells — a type of white blood cell that fights infections and cancer cells.
Targeting and blocking this interaction has been shown to promote T-cell activation, and to be associated with a protective effect against infections.
However, the potential role of PD-L1/PD-1 interaction in CF, and especially in CF patients infected by P. aeruginosa, remains unexplored.
Researchers in Madrid evaluated the levels of PD-L1 and PD-1 in CF patients, and the potential association between PD-L1/PD-1 interaction and P. aeruginosa infection.
The team analyzed the levels of PD-L1 in monocytes — a type of white blood cell that is in the frontline of infection, and communicates with T-cells — and of PD-1 in T-cells of 32 CF patients, 19 of them infected by P. aeruginosa, and of healthy volunteers. These cells also were grown in the lab to assess their proliferation and immune responses.
Results showed that CF patients had significantly higher levels of PD-L1 in monocytes and PD-1 in T-cells than healthy people, and that PD-L1 levels — both in monocytes and in a soluble form in the blood — were even higher in CF patients infected with P. aeruginosa.
These data, combined with the fact that CF patients infected with P. aeruginosa also showed a significant impairment in T-cell proliferation, highlighted an association between P. aeruginosa infection and an increased suppression of T-cells.
In accordance, additional analysis showed that endotoxin tolerance in monocytes was stronger in CF patients infected with P. aeruginosa than in those who were not.
Interestingly, the addition of an antibody that blocks PD-L1/PD-1 interaction to T-cells from patients infected with the bacteria significantly increased the proliferation of T-cells to levels almost comparable to those of healthy people and patients without the infection, suggesting this type of approach could revert the impaired immune response and benefit these CF patients.
The team also found evidence strengthening the hypothesis that bacteria/LPS presence in the blood induces increased levels of PD-L1 and endotoxin tolerance, as the levels of PD-L1 in monocytes from healthy people were significantly increased when in contact with isolated LPS of P. aeruginosa, or with blood of CF patients infected with the bacteria.
This PD-L1 increase with blood of infected CF patients was reduced when monocytes were pretreated with colistin (polymyxin E), a potent antibiotic that neutralizes or absorbs LPS. CF patients treated with colistin had lower levels of soluble PD-L1 in their blood.
These results suggest that colistin could be used to reduce the effects of bacteria passage to the bloodstream in CF patients infected with P. aeruginosa. Nonetheless, the team noted that future clinical trials are needed to confirm this hypothesis.
Overall, based on the results, the team concluded that “Pseudomonas aeruginosa colonization in patients with CF was associated with PD-L1 overexpression and impaired T-cell response, and LPS from this pathogen induced the observed phenotype.”
“Altogether, our results suggest the possibility of studying antibiotics and antiPD-1/PD-L1 antibody combination as a new potential treatment to provide clinical benefits to patients with P. aeruginosa colonization,” the researchers added.