Common P. aeruginosa Mutations May Lead to Biofilm Growth, Bacterial Persistence, Study Says
The common mutations that cause Pseudomonas aeruginosa to lose their ability to move are associated with a higher production of two complex sugar molecules implicated in the formation of biofilms — slimy layers of microorganisms that stick to wet surfaces and protect them from antibiotics and the host’s immune response, a study has found.
These mutations take place during chronic lung infections in cystic fibrosis (CF) patients, and this metabolic adaptation may be a new advantage for the loss of motility in these bacteria, which was already thought to be associated with two other benefits contributing to their persistence in CF airways.
The study, “Elevated exopolysaccharide levels in Pseudomonas aeruginosa flagellar mutants have implications for biofilm growth and chronic infections,” was published in the journal PLOS Genetics.
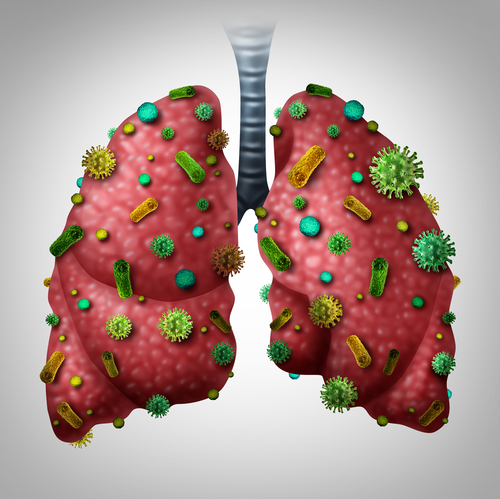
The characteristic buildup of thick mucus in CF patients’ lungs increases their vulnerability to respiratory infections, with the most common being those caused by the opportunistic bacterium P. aeruginosa.
P. aeruginosa is known to acquire a number of mutations thought to help in their long-term persistence during chronic lung infections. One of the most reported mutation-associated adaptation during these infections is the loss of the flagellum, a tail-shape structure that allows bacteria to move.
Current interpretations for flagellum loss in these bacteria include an immune advantage — as this structure’s main component triggers an immune response — and a metabolic benefit because these bacteria may have a higher growth rate without the energetic cost of producing a flagellum.
Scientists thus hypothesize that these advantages could lead to the evolution of non-flagellated bacteria during infection.
Now, a collaborative study between researchers in the U.S. and Canada identified a new potential benefit associated with flagellum loss in P. aeruginosa: the increased production of Pel and Psl, two key components of biofilms.
These complex sugar molecules are associated with antibiotic resistance and evasion from the host’s immune system. Notably, the presence of a P. aeruginosa variant producing higher-than-normal levels of Pel and Psl — known as rugose small colony variant (RSCV) — in CF patients’ sputum was previously linked to poor outcomes.
The team first conducted a screen for mutations associated with the RSCV, which identified mutations in 22 genes classified into four groups based on their functions. To the researchers’ surprise, 15 of these genes were associated with flagellum structure and function, which they decided to explore further.
When analyzing Pel and Psl production in non-flagellated RSCV bacteria grown in a liquid culture and in a solid medium, the team found that overproduction of these complex sugars only occurred when the bacteria were in contact with a surface (solid medium).
This suggested that surface contact might be a stimulus for non-flagellated mutants to produce biofilm-associated sugar molecules.
“These observations are consistent with reports that the flagellum has a role in mechanosensation [the ability to detect and respond to mechanical stimulus] that is similar to other bacteria,” the researchers wrote, adding that flagellum loss was previously shown to promote biofilm production in Vibrio cholerae, the bacteria that cause cholera.
In agreement, the researchers found that higher Psl levels required flagellar genes and components of a surface-sensing system. While the underlying mechanism of this association remains largely unclear, a possible explanation is that impaired function of flagellum components promotes signals that lead to biofilm formation, the team noted.
“These observations might be informative to our understanding of the early stages of biofilm formation,” the researchers wrote.
Further analyses revealed that these non-flagellated mutants rapidly increased in frequency in laboratory P. aeruginosa biofilms and that Pel and Psl production provided the main advantage in this environment.
Moreover, the team also identified non-flagellar P. aeruginosa associated with an RSCV behavior in samples from CF patients.
“We propose that loss of the flagellum may lead to biofilm growth that contributes to increased bacterial persistence during infection,” the researchers wrote, noting that this may be a new, non-exclusive, interpretation of the benefits of flagellum-associated mutations.