Stem Cell Therapy and Cystic Fibrosis: Embryonic and Induced Pluripotent Stem Cells
Written by |
Since I’ve started writing for Cystic Fibrosis News Today, I’ve received many messages and e-mails regarding the state of stem cell research and its impact on cystic fibrosis. Unfortunately, responding to these questions usually opened doors to more questions that could lead to some confusion. In order to confront the vast number questions concerning cystic fibrosis research, stem cells, and regenerative medicine, my next few articles will explore one aspect of cell therapy and CF.
There are several approaches that hold promise to improving the health and quality of life of CF patients. Current therapeutic methods have shown some success when treating symptoms, such as the use of antibiotics, advancements in airway clearance technology, inflammation, pancreatic enzymes, and CFTR correction drugs. However, new approaches can only improve our understanding of CF disease development and increase the current options to confront symptoms and disease progression. The use of stem cells plays a critical role in cystic fibrosis research, and could one day repair the damage accumulated by infection or replace cells with the defective CFTR protein.
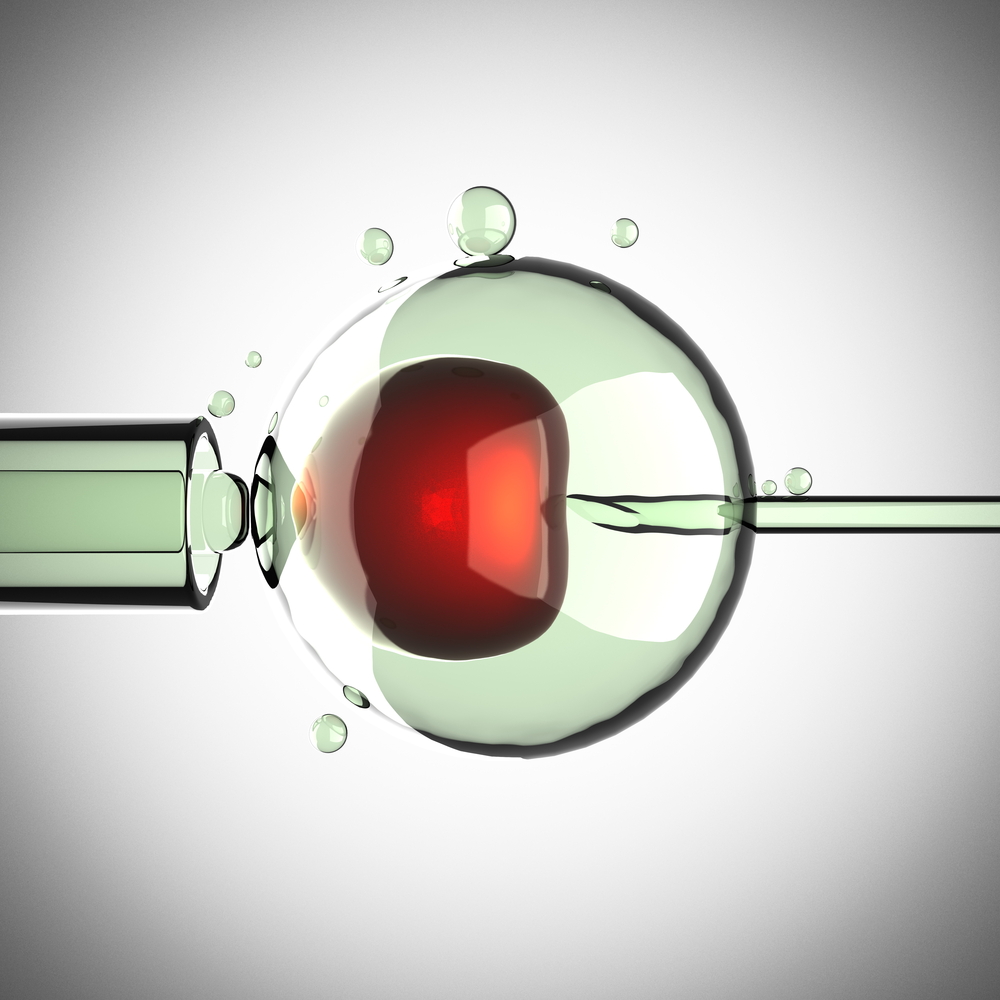
Perhaps the most commonly known type of stem cell is the human embryonic stem cell (ESC). Since these cells are pluripotent, they are particularly attractive because they have the ability to grow and remain stem cells, while also having the ability to differentiate into many cell types including lung and pancreatic cells. Because of this amazing ability, ESCs have been approached as a powerful form of study for diseases like cystic fibrosis. In fact, studies have shown that these cells may be able to repair and correct the defective CF cells within the lungs of mice tested in the lab.
Unfortunately, there remain several limitations of the therapeutic application of ESCs in patients with cystic fibrosis. Due to the source of the ESCs, therapy would require immunosuppression medications to avoid rejections. Also, the potential for these ESCs to form tumors in vivo poses a great threat to patients when these cells are used as a form of cell therapy. Because of these drawbacks, ESCs will likely serve as a better platform for drug testing to understand cystic fibrosis.
Another ethical shortcoming of embryonic stem cells is their cell source: human embryos. To bypass the ethical issues surrounding ESCs, the study of induced pluripotent stem cells (iPSCs) was born. Similar to ESCs, IPSCs show a great potential for disease modeling and testing, but unlike ESCs, IPSCs do not induce the same immune response and therefore would not require immunosuppressants. Instead of coming from the embryo, IPSCs come from easily accessible human tissues and are then transformed into a similar pluripotent stem cell state. With the development of methods to generate multiple cells types from iPSCs, future studies may investigate CFTR mutations in organs affected by the disease.
The field of iPSCs shows promise to become a powerful tool for understanding CF progression and developing new treatments, and is one major component of how stem cells may one day make a significant impact on treating cystic fibrosis.






