Arthritis Treatment Seen to Ease Inflammation and Lung Damage in Cystic Fibrosis
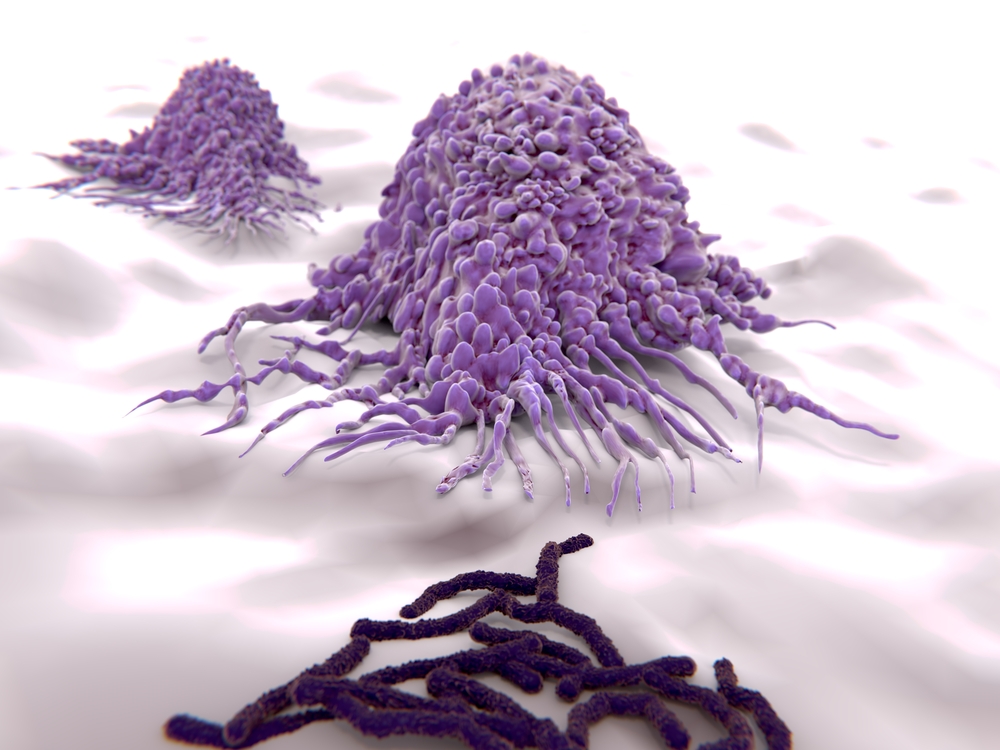
Abnormal activation of inflammasomes, complexes that lead to the production of pro-inflammatory molecules in response to a pathogen, often contributes to respiratory infections and pathologic airway inflammation. In a recent study, Italian researchers looked at how two distinct inflammasomes, NLRC4 and NLRP3, participate in cystic fibrosis (CF)-associated lung infections, showing that NLRP3 contributes more actively to harmful inflammatory responses.
The study, “IL-1 receptor antagonist ameliorates inflammasome-dependent inflammation in murine and human cystic fibrosis,” published in the journal Nature Communications, also found that NLRP3 activity can be impaired by Kineret (anakinra), an approved rheumatoid arthritis treatment, revealing a promising therapy approach for CF patients.
In CF patients, a continuous cycle of infection, inflammation, and tissue damage is responsible for the progressive decline of pulmonary function. When an infection takes place, the innate immune system is the first to be activated. This immune response relies mainly on cells that are always present, and ready to mobilize and fight microbes at the site of infection.
But the pulmonary innate immune response in CF is dysregulated at several levels, resulting in inefficient bacterial clearance and, ultimately, contributing to lung diseases associated with CF. Inflammasome activation is critical to fight infection, leading to the production of Interleukin (IL)-1β and IL-18 that recruit T-cells to kill the pathogens. But excessive activation of these complexes can result in an extreme inflammatory response that compromises the host’s ability to control infection.
Several different inflammasome complexes have been described to date. All of them recognize specific danger signals, and subsequently instruct immune cells to act against harmful pathogens.
To understand the role of NLRP3 and NLRC4 inflammasomes in CF, the team from University of Perugia infected CF mice with Aspergillus fumigatus and Pseudomonas aeruginosa, two common pathogens in CF patients.
Results revealed that both inflammasomes are involved in pathogen clearance, but NLRP3 was more commonly associated with harmful inflammatory responses in CF than NLRC4. This NLRP3-dependent response was particularly evident when the NLRC4 response was absent, suggesting that the production of an interleukin-1 receptor (IL1-R) antagonist by the NLRC4 pathway could be impairing NLRP3.
Consistently, the researchers found that inhibiting the IL-1β signaling with the approved IL-1R antagonist Kineret could improve the harmful effects of NLRP3. In fact, CF mouse models treated with Kineret showed significantly increased survival to P. aeruginosa infection, and lessened bacterial burden, neutrophil (a type of innate immune cell) recruitment, and lung damage.
These findings suggest that Kineret may be a promising approach to reduce the infection and inflammation-derived lung damage in CF patients.
“In conclusion, our study shows that the elucidation of pathogenic, inflammasome-dependent mechanisms at the molecular level may help the development of novel strategies for patient stratification and personalized tailored approaches in human CF,” the authors wrote.