Yeast Models Suggest New Ways of Restoring CFTR Function in Lungs of CF Patients
Written by |
Researchers partially restored the function of the CFTR protein in lung cells isolated from cystic fibrosis (CF) patients by blocking a particular protein involved in its translation. The findings were published in the journal PLOS Biology, in the study “Ribosomal Stalk Protein Silencing Partially Corrects the ΔF508-CFTR Functional Expression Defect.”
CF is a genetic disease characterized by persistent lung infections and difficulty in breathing, due to mucus build up in the lungs. Healthy lungs produce mucus that is transported to the throat by the waving movements of ciliated cells in the respiratory tract, helping to remove small particles, including bacteria or viruses, that have been inhaled. In CF patients, however, a defect in the CFTR chloride channel causes the mucus to thicken, preventing its clearance.
The most common CF mutation, ∆F508-CFTR, is known to affect 90 percent of CF patients, half of whom have two copies of this mutation. It induces the substitution of one amino acid that interferes with the protein’s correct folding and leads to its degradation.
Researchers at the University of Alabama at Birmingham (UAB), along with colleagues at Emory University, Atlanta, and McGill University, Canada, used a yeast genetic model to find novel therapeutic targets for CF patients with this mutation.
“We are curious about the extent to which yeast genetic models can reveal gene interaction networks relevant to human disease,” said John L. Hartman IV, MD, an associate professor in the UAB Department of Genetics and the Gregory Fleming James Cystic Fibrosis Research Center, in a press release. “For cystic fibrosis, this yeast phenomics approach appears to be very useful.”
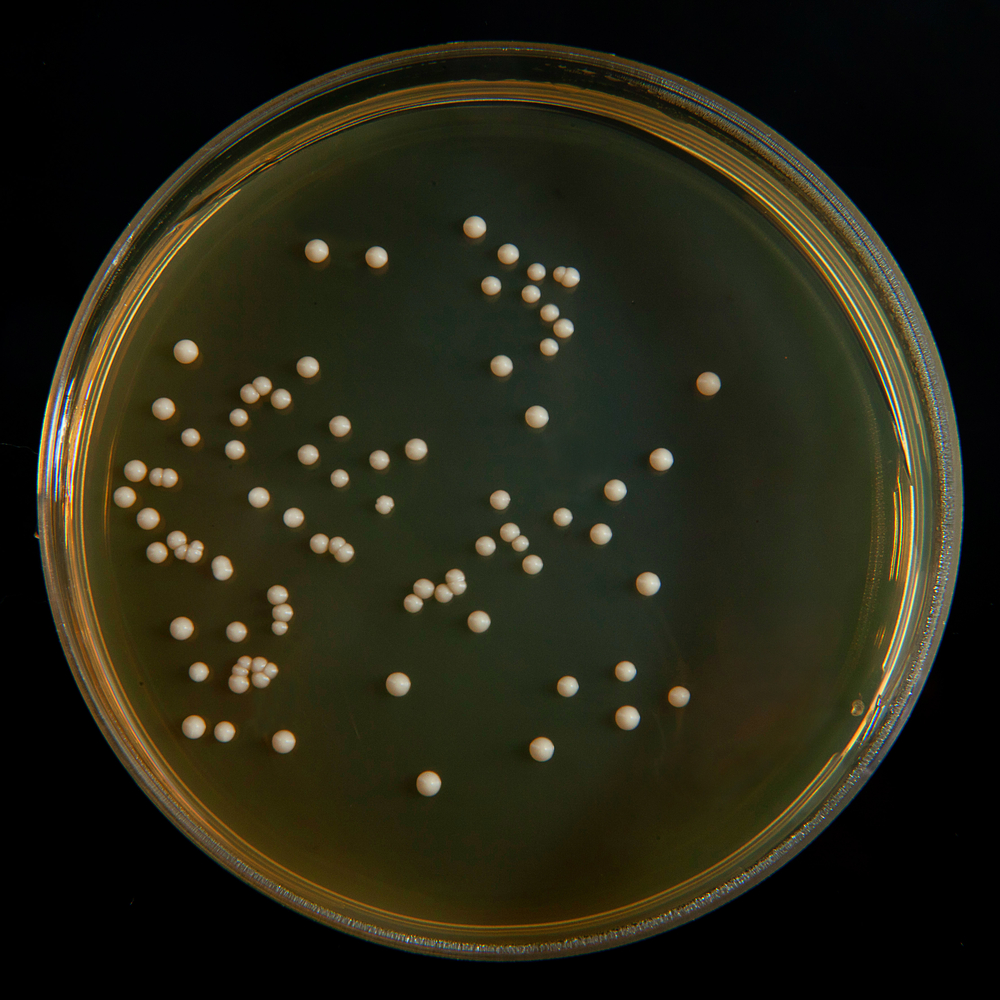
Yeast has a homolog gene to CFTR, called YOR1, which works as a pump for the mitochondrial toxin oligomycin, making the yeast resistant to oligomycin. YOR1 has an equivalent mutation to the human ∆F508-CFTR, known as ∆F670-YOR1; this mutation, like its human counterpart, also leads to misfolding and degradation. The researchers introduced ∆F670-YOR1 in approximately 4,700 different yeast strains, with a depletion of a single yeast gene. This enabled the team to find new targets that rescued the folding problems of the mutated protein by measuring changes in oligomycin resistance in yeast.
A number of genes were identified as potential targets that were able to restore ∆F670-YOR1 folding and prevent degradation, suggesting that their human homologs would also rescue ∆F508-CFTR activity. To test them, the investigators suppressed the levels of the corresponding human proteins, using an interfering RNA approach in human bronchial epithelial cells isolated from CF patients who carried the ∆F508-CFTR mutation.
RPL12 inhibition, particularly, was found to increase ∆F508-CFTR density at the plasma membrane of these cells, as well as its function and stability.
RPL12 is a protein involved in the translation of mRNA into protein, and its suppression slows the rate of CFTR translation, possibly reducing the amount of misfolded proteins during synthesis. When RPL12 inhibition was combined with the small molecule corrector VX-809 (lumacaftor), a molecule that can directly bind and promote the folding of ΔF508-CFTR, the CFTR function in CF cells was restored to 50 percent of what is found in normal bronchial epithelial cells, which is above the threshold required for healthy lung function.
“The research is the first preclinical study, to our knowledge, that demonstrates therapeutic levels of ∆F508-CFTR function in primary patient cells,” said Dr. Hartman.
This work also provides the first evidence that novel therapeutic CF targets may be identified based on yeast studies, due to the high functional conservation between some yeast and human genes.