Low-dose Nitric Oxide Enhances Antibiotic Treatment of Certain Chronic CF Infections
Written by |
Nitric oxide (NO) inhalation can enhance the antibiotic treatment of Pseudomonas aeruginosa biofilm infections in cystic fibrosis (CF) patients, a small proof-of-concept clinical trial demonstrated.
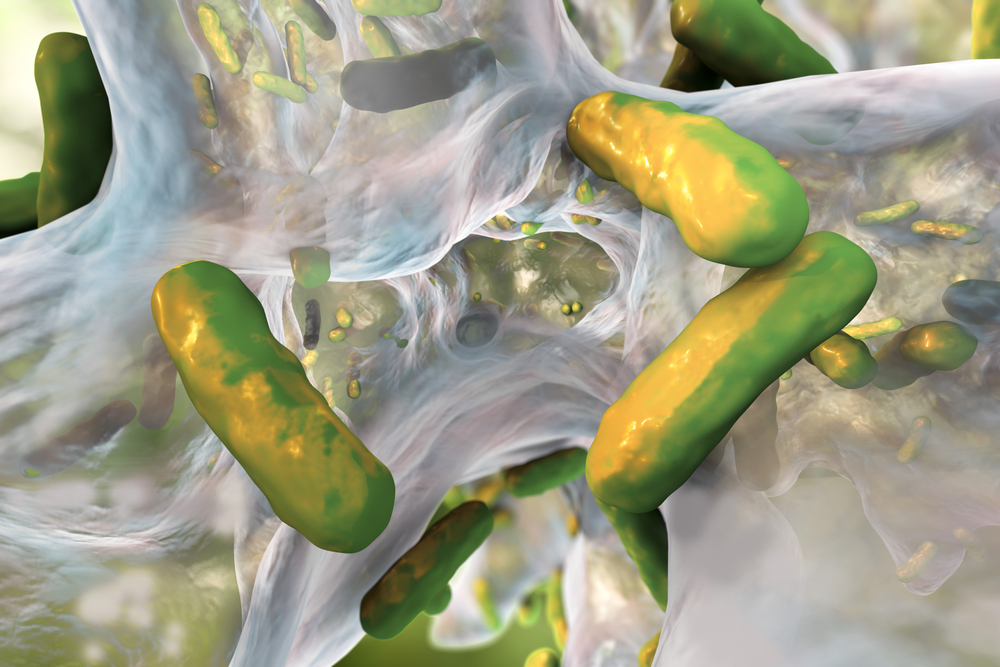
Bacterial infections by P. aeruginosa is a major cause of long-term morbidity and mortality in patients with CF. The bacteria can form biofilms, which are structured, antibiotic-tolerant aggregates that form in the lungs of patients. They can form either as aggregates in the mucus of a CF lung or attach to lung tissue, and are difficult to remove using conventional therapeutic methods.
Biofilms can increase bacterial tolerance to antibiotics by 1,000-fold, in addition to resisting the patient’s immune system responses. Therefore, there is a need for new approaches to target biofilm infections.
The authors of the study, “Low-Dose Nitric Oxide as Targeted Anti-biofilm Adjunctive Therapy to Treat Chronic Pseudomonas aeruginosa Infection in Cystic Fibrosis,” published in the journal Molecular Therapy, had previously shown that NO can disperse P. aeruginosa biofilms.
In the current study, they demonstrate the nitric oxide effect on biofilms from CF patient sputum samples (ex vivo) and in a proof-of-concept clinical trial.
P. aeruginosa biofilms in sputum samples from CF patients were dispersed within five to 10 hours of nitric oxide treatment at low concentrations (less than 500 nM). When the researchers compared antibiotic treatment of the biofilms with a combination of antibiotics plus NO, they found that the combination significantly reduced mean biofilm biomass and thickness.
In fact, treatment with the antibiotic tobramycin alone (without nitric oxide) increased the biofilm biomass and thickness by 243 percent and 199 percent respectively, compared to non-treated biofilms.
Following this significant finding of the importance of adjunctive nitric oxide use, researchers performed a proof-of-concept clinical trial to demonstrate the effect in patients.
All 12 patients received conventional intravenous antibiotic therapy. The test group also received low-dose nitric oxide (through inhalation), while the control group received a placebo. The results showed that over the seven days of treatment, biofilms were significantly reduced in patients receiving NO compared to those receiving antibiotics alone.
No side effects were detected and the treatment did not cause an increase in acute exacerbations.
Although the researchers admit that the small sample number and the design of the study pose certain limitations, they state that it provides a proof-of-concept.
“Our results suggest a benefit of using low-dose NO as adjunctive therapy to enhance the efficacy of antibiotics used to treat acute P. aeruginosa exacerbations in CF,” the team wrote. “Strategies to induce the disruption of biofilms have the potential to overcome biofilm-associated antibiotic tolerance in CF and other biofilm-related diseases.”
“Biofilm-related chronic infections are responsible for at least half a million deaths per year at an estimated cost of over $94 billion in the United States alone,” they added. “More effective anti-biofilm therapies are needed to address this significant unmet need.”






