Manuka Honey Could Be Used to Treat CF Lung Infection P. Aeruginosa, Study Suggests
Written by |
Manuka honey, produced from the nectar of a flowering plant native to Australia and New Zealand, showed significant anti-Pseudomonas aeruginosa activity in an experimental model of lung infection designed to closely replicate the pulmonary environment of patients with cystic fibrosis (CF).
The results were reported in the study “Anti-pseudomonad Activity of Manuka Honey and Antibiotics in a Specialized ex vivo Model Simulating Cystic Fibrosis Lung Infection,” published in the journal Frontiers in Microbiology.
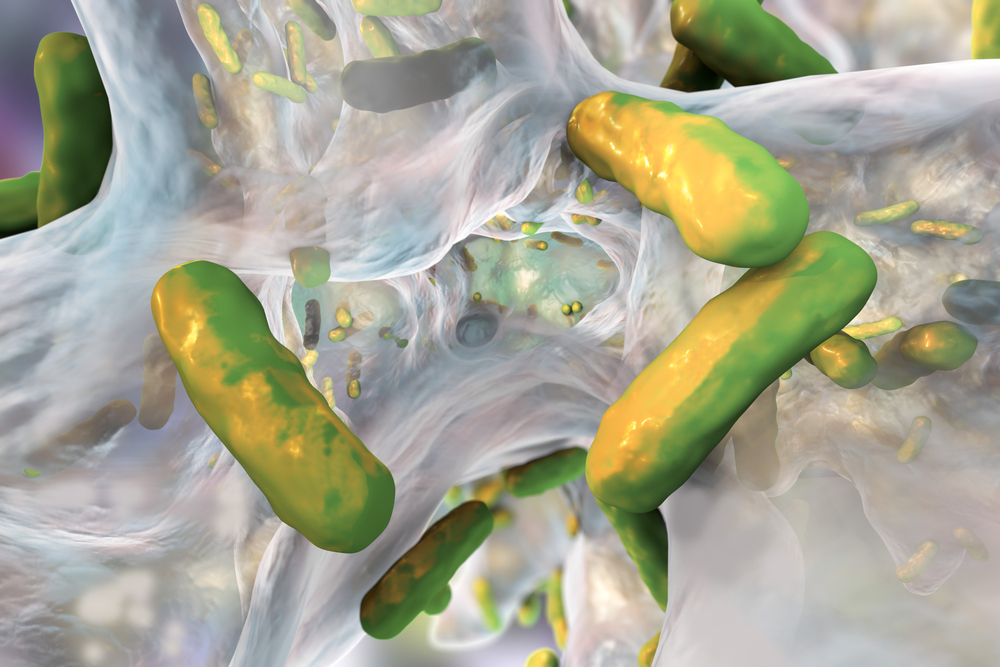
Up to 80% of CF patients are infected at some point with P. aeruginosa bacteria. This pathogen has innate and acquired antimicrobial resistance mechanisms, and the ability to form biofilms — a slimy substance in which bacteria stick to each other, allowing them to resist the action of antibiotics and the immune response.
As a result, it is not always possible to eradicate P. aeruginosa from CF lungs, even with aggressive antimicrobial treatment regimens. Many patients harbor multidrug-resistant strains, and infection is linked to a poor prognosis and persistent infection. That is why antimicrobial agents with anti-biofilm effects are urgently needed.
For decades, medicinal (sterilized) manuka honey has been used successfully to treat chronically infected surface wounds, and it has shown exceptional activity against a range of antibiotic-resistant microorganisms. Manuka honey, for instance, can disrupt the cell envelope of P. aeruginosa.
Ask questions and share your knowledge of Cystic Fibrosis in our forums.
Manuka honey is monofloral, meaning that it is produced from the nectar of a single plant species — the manuka tree (Leptospermum scoparium). The antibacterial activity of manuka honey is due to the abundant presence of a compound called methylglyoxal (MG). MG is found in most types of honey, but only in small quantities.
Scientists tested the antimicrobial activity of manuka honey against 28 different P. aeruginosa isolates associated with CF infection. They compared it with three clinically relevant antibiotics: ciprofloxacin, ceftazidime, and tobramycin, alone or in combination.
Antimicrobial activity was measured in two ways: by conventional antimicrobial susceptibility testing (AST, which is what clinical labs routinely do), and by using two ex vivo porcine (pig) lung (EVPL) models, which use resected fragments of alveolar and bronchiolar tissue to better replicate the pulmonary environment.
In AST experiments, most P. aeruginosa isolates were sensitive to tobramycin (20 out of 28), but were resistant to ciprofloxacin (17 of 28) and ceftazidime (15 of 28). In contrast, all isolates were inhibited by 16% or 32% by manuka honey concentration. Four of the isolates were resistant to all the antibiotics tested, but were inhibited by manuka honey.
However, the combination of sub-inhibitory manuka honey and antibiotics had no effect against most tested isolates.
Using the two ex vivo porcine lung models, 64% manuka honey inhibited many of the isolates, whereas abnormally high concentrations of antibiotics could not. The combination of manuka honey and antibiotics showed increased antimicrobial activity in these models —90% of the bacteria tested were killed.
“The preliminary results are very promising and should these be replicated in the clinical setting then this could open up additional treatment options for those with cystic fibrosis infections,” Rowena Jenkins, PhD, senior author of the study and lecturer in microbiology and infectious diseases at Swansea University, U.K., said in a press release.
A limitation of this discovery, the team noted, is the difficulty in delivering manuka honey deep inside the lungs of patients. Nebulization may not work because it is unlikely that the required concentrations would reach the affected tissues. According to the researchers, “concentrations in the region of 40% [weight/volume] could be achievable; however, efficacy at this concentration needs to be experimentally tested.”
A more immediate application could be manuka honey incorporated into a sinus rinse solution to clear sino-nasal cavity infection reservoirs, preventing the migration of bacteria from the upper airway into the lungs. Swansea University is sponsoring a clinical trial to test this approach.
“The synergy with antibiotics and absence of resistance seen in the laboratory has allowed us to move into the current clinical trial, investigating the potential for Manuka honey as part of a sinus rinse for alleviating infection in the upper airway,” Jenkins said.






