Healthier Ways to Help Gain Weight
Written by |


Gaining weight can be just as difficult as maintaining lung function for many with cystic fibrosis. Most have heard people without CF joke that they wish they had our problem with gaining weight. But for those who experience the struggle of malnourishment and unstable weight, we know it isn’t all giggles and gluttony.
Between infections and heavy breathing burning loads of calories, nausea and poor appetite keeping us from eating, and conditions like pancreatic insufficiency and diabetes getting in the way, it’s a tough journey to get to that ideal body mass index (BMI).
It would be nice to just remain thin without problem, but we know there is a strong correlation between BMI and lung function. Before you jump to just eating junk food, troubleshoot for stomach problems or optimize your current regimen.
Here are some tips from my lifetime of chasing weight gain:
If the tests don’t hurt, might as well do them.
There is a very long list of conditions that are common for those with cystic fibrosis and could affect weight gain: diabetes, celiac disease, gastroesophageal reflux disease (GERD), gastroparesis, motility disorders, C. Diff., H. Pylori, constipation, diarrhea. With so many general GI problems, it’s often difficult for a CF patient to notice new symptoms. Thankfully, many of these conditions are diagnosed with painless testing (other than the humiliation of having to collect stool).
I recommend seeing a gastrointestinal (GI) doctor with CF experience rather than relying only on your CF doctor to make these particular diagnoses. The tummy is their specialization, while CF doctors specialize in pulmonary problems.
Optimize your supplementation.
CF weight gain for those with pancreatic insufficiency isn’t as easy as simply eating more. We often require extra help in the form of pancreatic enzymes, probiotics, anti-nausea medications and remedies, and calorie-packed tube feeds.
For years, I accepted the gastrostomy tube (G tube) as the best option for packing in extra calories, protein, and fat thanks to my crippled appetite. But this caused extreme nausea and reflux, which led to aspiration damage in my lungs. About a year ago, I got a gastrostomy-jejunostomy tube (G-J tube), which sticks into both my stomach (G) and small intestine (J). I mostly just used the J part, which ended reflux and nausea caused by the tube feedings — it bypasses the stomach, which is where my nausea and reflux boiled.
Many don’t get J tubes because, historically, they’ve stuck out a lot more. Now, though, there are low-profile tubes that you can’t see through the shirt. I also still have the G part, which means I can inject medications into the stomach if I can’t take them by mouth for whatever reason.
I’ve also seen success in changing my pancreatic enzyme brand (such as using Relizorb for tube feeds — a game changer), my anti-nausea medication, anti-reflux medication, and probiotic strains. Ask your doctor if they believe changing brands, medication types, or strains could positively affect your absorption of nutrients.
Change how and what you eat.
Change the way your brain thinks about food. Counting calories works for some and hinders others. If you want to try counting calories, free apps like MyFitnessPal and SparkPeople carry loggable nutritional information for a wide variety of foods and drinks. Remember to focus on not only calories, but fat and protein, too.
You can “trick” your brain and stomach into accepting more calories and fat by drinking smoothies and milkshakes, or by grazing throughout the day rather than eating big meals. Meal prep is effective for some: “By the end of the day, every scrap in this Tupperware must be gone.”
Here’s an example of a snack pack I prepared each day of a hiking trip I went on:
And here’s a simple, but yummy, three-ingredient smoothie recipe I blended: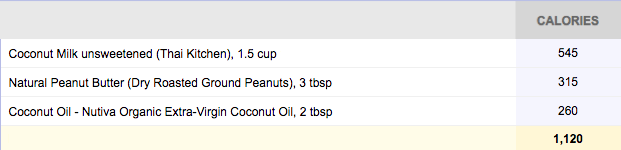
I know that “recipe” looks too basic to be good, but I swear it is!
Understand nutrition and your disease.
The best way to tackle a problem is to understand its cause and solutions. Look into the science of nutrition and CF-related GI problems to see how they affect each other. Know that not all weight is created equally; there’s muscle, fat, and water weight. Know not all fats are created equally; there are unsaturated, monounsaturated, polyunsaturated, trans fats, etc. You might never know as much as your nutritionist or GI doctor, but just learning the basics will help you think outside the box (and avoid common nutrition myths on the internet).
Ask your doctor to educate you or check out some of the following resources:
***
Note: Cystic Fibrosis News Today is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website. The opinions expressed in this column are not those of Cystic Fibrosis News Today, or its parent company, Bionews Services, and are intended to spark discussion about issues pertaining to cystic fibrosis.







Robert Eckheart
I have CF, and I struggle to maintain a weight I am happy with. I weigh about 145 pounds on a low day. I eat nearly 4,000 calories a day, and eating is a big priority for me. It isn't getting me anywhere though in terms of weight gain. Before the start of this previous Baseball season, I weighed in at 153 lbs. This was my highest weight ever. After running, and cardio through baseball my weight has gone down significantly. I just want to know the best ways in which I can gain weight. What foods can I eat specifically that will help me the most. I lift weights and gain all my weight through muscle it seems, and I live a very healthy lifestyle with my activeness. I want to know how I can gain fat. How can I get bigger with CF? Is it possible to reach my body weight goals, or am I sad out of luck? I didn't mention I am 17, and a Sophmore in High School. I attend Helen Devos Children Hospital in Grand Rapids MI.
Taylor Smith
Hey I’m 23 and my son is 1 he has CF and I can tell you some things that will help you that I give him