Money and Insurance Worries Deeply Affect CF Outcomes in US, Experts Say
Written by |
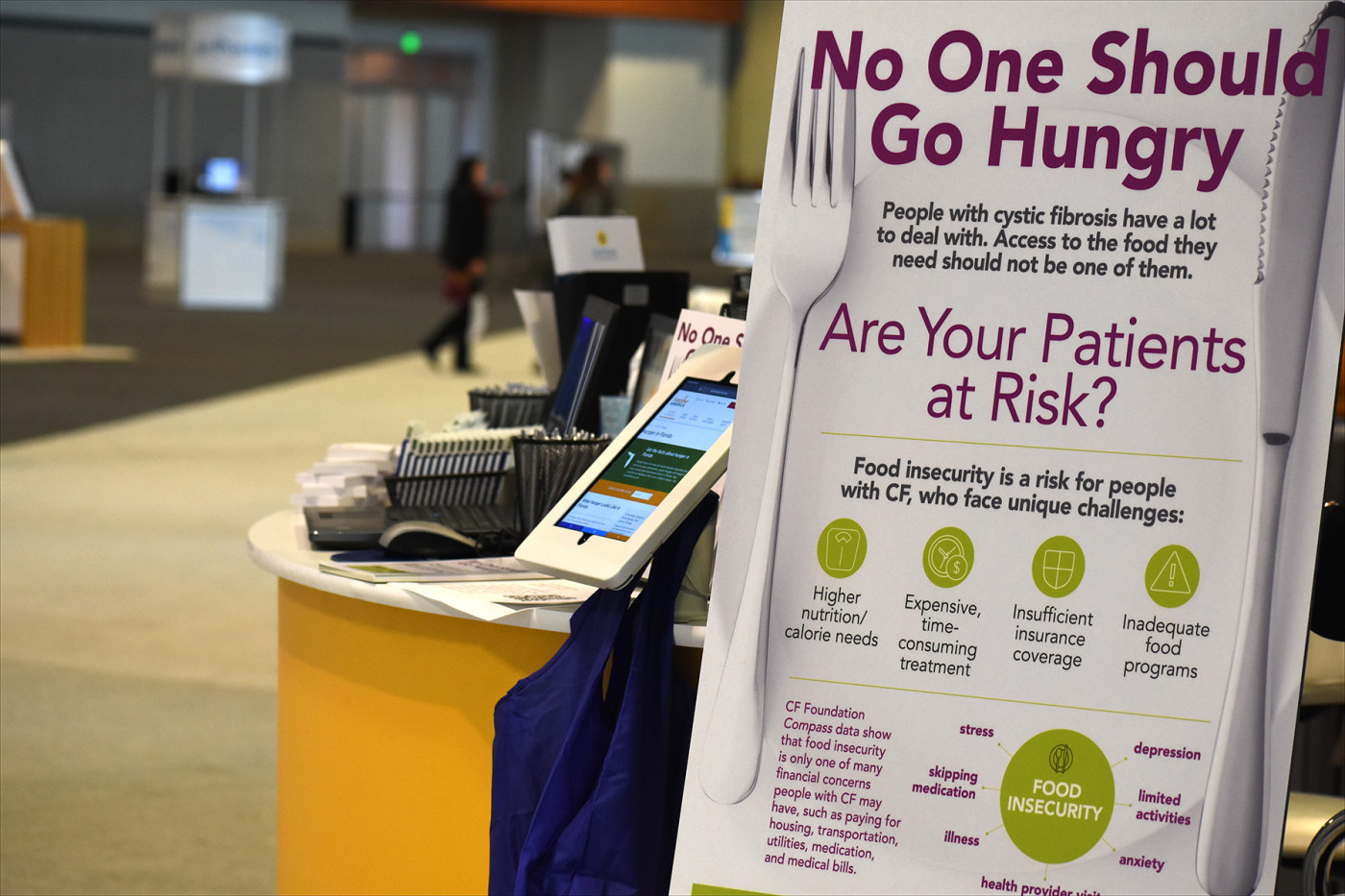
Cystic Fibrosis Foundation display at NACFC 2019. (Photo by Larry Luxner)
Income level is the greatest single determinant of well-being in people with cystic fibrosis in the United States, said experts at a recent CF conference.
Social worker Kim Reno, a manager at the Cystic Fibrosis Foundation’s Compass patient assistance program, estimates that actual healthcare determines only 20% of any given person’s level of health.
Socioeconomic status (income and education levels, occupation) accounts for 40%, health behaviors (diet, exercise, alcohol use, smoking, sexual activity, etc.) another 30%, and place of residence the remaining 10%.
“Evidence has shown that food and housing insecurity drives healthcare-related costs in the CF community,” she said. “People have also expressed concerns about health insurance, social support, living expenses, food expenses, and transportation. People with CF are more at risk because of the complexity of care that CF requires.”
Reno was among several speakers to address the economics issue during a panel at the 2019 North American Cystic Fibrosis Conference (NACFC) in Nashville.
The event attracted about 5,000 people, and came barely a week after the U.S. Food and Drug Administration’s approval of Trikafta — a combination therapy of elexacaftor, ivacaftor and tezacaftor developed by Vertex Pharmaceuticals — in October. Trikafta people with the most common CF-causing mutation, that of at least one F508del defect in the CFTR gene, found in an estimated 90% of all patients.
The 13 case managers who work at CFF Compass handled more than 7,000 calls from 6,400 individuals in 2018, Reno said. About 23% of all cases involved connecting families with financial resources.
“At CFF Compass, we seek to better understand the social factors people with CF and their caregivers have identified as challenging,” she said, noting that the most requests for help came from California, Texas, Florida, New York, and Ohio.
“We do help people regardless of their immigration status, but we’re limited to the resources that are available.”
Screening for honest answers
Gabriela Oates, PhD, led a study that electronically screened caregivers of kids with CF at the University of Alabama’s Pediatric CF Center in Birmingham. Participants were given encrypted iPads protected by Ziploc bags, and the questionnaires themselves screened for 10 unmet needs and associated stress levels.
One of the survey’s questions was: “Are you concerned that food will run out before you can buy more?”
According to Oates, “asking pediatric caregivers about sensitive topics may be more effective when not done face-to-face … They tend to answer questions honestly when digital screening is used.”
Oates found lung function to be 9% lower in Medicaid versus non-Medicaid patients, and 3% to 10% lower among those living in poorer neighborhoods. (Medicaid is a government-run insurance program for people with low incomes and for some with disabilities.)
“Medicaid patients are twice as likely or more to be in the fifth or lower percentile for weight and height,” she said. “Patients in economically deprived areas have lower BMI [body mass index], while the risk of chronic Pseudomonas aeruginosa infection is 1.9 times more likely, and MRSS-related [methicillin-resistant staphylococcal strains] infections 2.2 times more likely.”
Oates and her team screened 109 families over a three-month period from May to July 2019. She found their biggest concerns were money (32% of all respondents), followed health insurance and smoke exposure (28% each). Other factors that worried families affected by CF were food and housing insecurity (17%), availability of childcare (15%), and transportation (9%).
“Those who had concerns about running out of food were also concerned about housing and transportation,” she said. “We did see a significant association between money concerns and both ppFEV1 [a measure of lung function] and hospitalizations.”
Food or meds: Tough choice for some
Michael Schechter, MD, is a professor of pediatrics at Virginia Commonwealth University in Richmond. He says inadequate insurance coverage directly correlates with poorer FEV1 scores (forced expiratory volume in one second; a measure of lung function), based on a study that compared such scores with patients’ zip codes, and whether they had private insurance or depended on Medicaid.
“Patients with lower education and low socioeconomic levels may be less likely to recognize lapses in care, and feel less empowered to raise concerns or question treatment,” he said. “It is therefore plausible that efforts to improve the consistency of care will reduce disparities.”
Cynthia Brown, director of the Adult CF Program at Indiana University, said such disparities are likely to increase as CF patients live longer, and medications become more and more expensive.
“We have patients whose insurance coverage often lapses for long periods because they don’t understand the complexities, or they make just enough money to no longer qualify for Medicaid,” Brown said. “Their health is compromised because their care is interrupted.
“We also have patients who travel very long distances to get to their CF centers, and some patients who make an hourly wage have to choose between paying for food of paying for their prescriptions.”
Complicating the picture, said Terri Laguna, MD, is the fact that Trikafta treats the vast majority of those with CF, but not everyone.
“While this is truly an exciting time, don’t forget that not everyone with CF is going to qualify for a CFTR modulator. This means 10–20% of people with CF will still be essentially invisible. The approval of Trikafta has accentuated this disparity as people become more aware of their phenotype,” said Laguna, co-director of the Minnesota Cystic Fibrosis Program in Minneapolis.
“People with rare mutations also tend to be from under-represented minorities, such as African-Americans and Hispanics. Over half of those 20% who don’t qualify for Trikafta belong to an under-represented minority group,” Laguna said. “We see that you’re out there, and we won’t give up until you have a cure as well.”









