FAQs about Kalydeco
There are no known interactions between Kalydeco and alcohol. Patients are advised to speak with their healthcare team about whether it is safe to drink alcohol while on this medication.
Animal studies generally indicated no treatment-related adverse effects on the fetus or on offspring development with Kalydeco’s active component, except decreased fetal body weights at maternal doses above the maximum recommended human dose. However, data on pregnant women are limited. It is not known whether this treatment passes to human breast milk. Patients should inform their healthcare team if they are pregnant or plan to become pregnant, are breastfeeding, or plan to do so.
Neither hair loss nor abnormal weight gain have been reported as a side effect of Kalydeco. Patients who experience unanticipated effects after starting a new cystic fibrosis therapy are advised to talk to their healthcare provider.
Clinical trials testing Kalydeco in CF patients with a G551D mutation in the CFTR gene showed the treatment could lead to significant improvements in lung function, relative to a placebo, within 4 weeks compared to study start. However, each person may respond differently to treatment, thus patients are advised to discuss with their healthcare team how Kalydeco can help in their particular case.
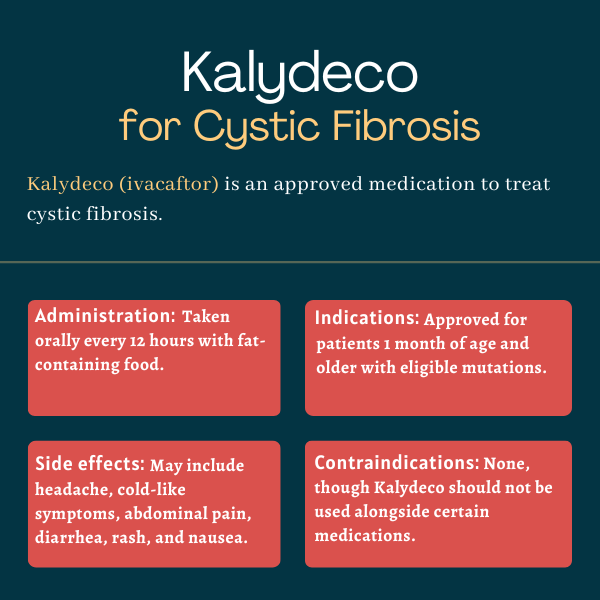
Kalydeco was approved by the U.S. Food and Drug Administration in January 2012 for cystic fibrosis (CF) patients, ages 6 and older, with at least one copy of the G551D mutation in the CFTR gene. This approval was later expanded multiple times, now covering children as young as 1 month with CF caused by one of 97 genetic mutations.
Related Articles

 Fact-checked by
Fact-checked by