New X-Ray “Blueprint” of Pseudomonas Aeruginosa May Lead To New Cystic Fibrosis Therapies
Written by |
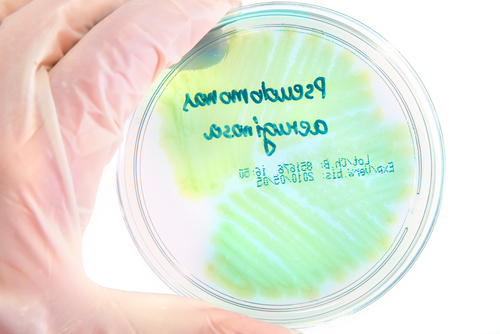
 Pseudomonas Aeruginosa is a complex, formidable bacterial infection that is notoriously difficult to treat, particularly in patients with lowered immune response and who have Cystic Fibrosis. While the bacteria’s mode of operation, which involves targeting and infecting damaged tissue, is relatively well understood, the method by which Pseudomonas Aeruginosa adapts to and avoids treatment — a product of its cellular makeup — has remained elusive to researchers. However, a study led by Trinity College Dublin scientists is shedding new light on the design and structure of the bacteria, which in turn will enable researchers to develop new therapies that combat the infection more effectively.
Pseudomonas Aeruginosa is a complex, formidable bacterial infection that is notoriously difficult to treat, particularly in patients with lowered immune response and who have Cystic Fibrosis. While the bacteria’s mode of operation, which involves targeting and infecting damaged tissue, is relatively well understood, the method by which Pseudomonas Aeruginosa adapts to and avoids treatment — a product of its cellular makeup — has remained elusive to researchers. However, a study led by Trinity College Dublin scientists is shedding new light on the design and structure of the bacteria, which in turn will enable researchers to develop new therapies that combat the infection more effectively.
The research team at Trinity used an imaging technique called X-ray crystallography to gain new insights into the cellular structure and machinery of the bacterium, thus creating a kind of structural “blueprint” that will aid scientists in pinpointing Pseudomonas Aeruginosa’s weaknesses. The imaging method was used by Dr. Martin Caffrey, a Professor of Membrane Structural and Functional Biology at Trinity, who has also helped in developing the use of the technology in the research field as well. X-ray crystallography is a next-generation, high-throughput imaging method that is offering researchers access to the vanguard of creating protein blueprints such as the one used in this new research effort, as the method is proven to be highly effective in creating detailed protein crystals.
[adrotate group=”1″]
Once Professor Caffrey rendered the protein crystal blueprints of Pseudomonas Aeruginosa, researchers at University of Oxford were able to plug these blueprints into dynamic computer simulations that depicted molecular docking procedures, thus revealing the opening and closing of specific pores in the bacteria’s cell membrane. Caffrey and colleagues noted in their observations that the opposite ends of these pores feature loops that lead to flexible gateways. Together with another key finding — a protein that exists between the cell membrane’s inner and outer surface, functioning as a kind of escort and shuttling alginate to corresponding gateways — these new insights could prove valuable in developing new treatment options.
Dr. Caffrey, who also served as a corresponding author for the study, which was published in Acta Crystallographica Section D, entitled, “A conformational landscape for alginate secretion across the outer membrane of Pseudomonas aeruginosa,” recently explained in a press release that, “If we can knock out the functioning of this pore, we might be able to stop alginate being added to the troublesome biofilm. Blocking the release of this virulence factor is likely to weaken the bacterium, which should make it more susceptible to host defences.”
What makes Caffrey’s new imaging and understanding of Pseudomonas Aeruginosa so encouraging for Cystic Fibrosis patients is that the new insights gained from this fresh look into how the bacteria behaves can specifically aid drug developers in improving therapies that target its viscous biofilm, which serves as a robust defense mechanism and is traditionally very difficult to penetrate. Because alginate is a significant contributor to the resilience of the biofilm, being able to now therapeutically focus on the function of the pores where alginate exits the membrane could allow new drugs to kill Pseudomonas Aeruginosa more efficiently.