Study Finds Interferon Gamma (IFN-y) Immune Stimulation Helps Clear Lethal B. cenocepacia in CF Patients
Written by |
 A new study led by a team in the Research Institute at Columbus, Ohio based Nationwide Children’s Hospital and published in the journal PLoS One this month, suggests that boosting a key immune process called autophagy a natural process in which proteins and other cell materials are degraded and disposed with interferon gamma (IFN-y), could help clear a lethal bacterial infection in cystic fibrosis (CF).
A new study led by a team in the Research Institute at Columbus, Ohio based Nationwide Children’s Hospital and published in the journal PLoS One this month, suggests that boosting a key immune process called autophagy a natural process in which proteins and other cell materials are degraded and disposed with interferon gamma (IFN-y), could help clear a lethal bacterial infection in cystic fibrosis (CF).
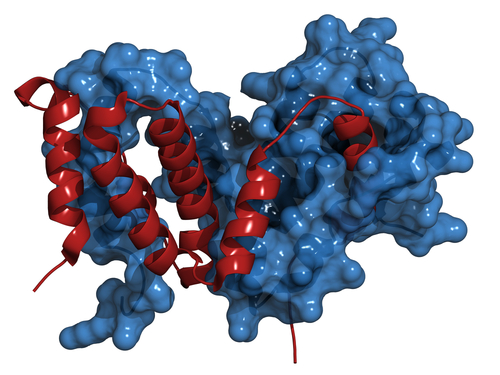
Autophagy is defective in CF but can be stimulated in murine CF models leading to increased clearance of B. cenocepacia, but little is known about autophagy stimulation in human CF macrophages. However, since IFN-y activates macrophages and increases antigen presentation while also inducing autophagy in macrophages, the researchers therefore hypothesized that treatment with IFN-y would increase autophagy and macrophage activation in patients with CF.
Cystic fibrosis is caused by a malfunction in the CFTR gene, which is responsible for transporting chloride and water across cell membranes. In people with the disease, cells that line the passageways of the lungs, pancreas and other organs produce unusually thick and sticky mucus that clogs airways and creates a hospitable environment for pathogens such as the pathogenic bacterium Burkholderia cenocepacia.
A member of the Burkholderia cepacia group of bacteria, B. cenocepacia is commonly found in soil and water, and in most instances poses no health threat to most of the population. However, in two to five percent of CF patients, the bacterium causes infection that can spread to the bloodstream, potentially triggering a general inflammation (sepsis) that can be fatal. Unhappily, B. cenocepacia doesn’t respond to most antibiotics, leaving physicians few weapons with which to fight it, and even if their infection isn’t severe, patients with B. cenocepacia are considered poor candidates for the lung transplant, which that many advanced CF patients require to survive.
[adrotate group=”1″]
 “B. cenocepacia is multi-drug resistant, so usually when patients are ill, they are on a cocktail of antibiotics and we’re hoping for a synergy of effect,” says Benjamin T. Kopp, MD, a pulmonologist at Nationwide Childrens, and a principal investigator for the Nationwide Children’s Center for Microbial Pathogenesis microbial-pathogens, an institution whose mandate is to develop greater understanding of molecular mechanisms by which microorganisms cause infectious diseases, as well as how the host responds to these disease states.
“B. cenocepacia is multi-drug resistant, so usually when patients are ill, they are on a cocktail of antibiotics and we’re hoping for a synergy of effect,” says Benjamin T. Kopp, MD, a pulmonologist at Nationwide Childrens, and a principal investigator for the Nationwide Children’s Center for Microbial Pathogenesis microbial-pathogens, an institution whose mandate is to develop greater understanding of molecular mechanisms by which microorganisms cause infectious diseases, as well as how the host responds to these disease states.
Further complicating these infections, Dr. Kopp notes, is that B. cenocepacia can replicate inside macrophages, the immune system’s first line of defense against microbial pathogens. It can avoid the host immune response, he observes, and is where something like IFN-y might work better than traditional antibiotics.
Dr. Koop is senior and corresponding co-author of the study “IFN- Stimulates Autophagy-Mediated Clearance of Burkholderia cenocepacia in Human Cystic Fibrosis Macrophages” (Published online May 05, PLoS One. 2014 May 5;9(5):e96681. eCollection 2014. www.plosone.org/article/info%3Adoi%2F10.1371%, DOI: 10.1371/journal.pone.0096681), co-authored by Kaivon Assani, Mia F. Tazi, and Amal O. Amer.
Produced by the IFNG gene in humans, IFN-y is a cytokine active in the immune system. Earlier studies suggested that the molecule stimulates autophagy, noting that in many diseases, including CF, autophagy is inhibited. Dr. Kopp and his colleagues wanted to see if treatment with IFN- might activate autophagy, allowing the body’s immune system to battle B. cenocepacia.
The researchers isolated macrophages from patients with and without CF and infected them with B. cenocepacia in cell cultures. When they analyzed the samples, they found that the cells from CF patients had decreased levels of IFN-y. They then treated the CF macrophages with synthetic IFN-y and found that autophagy was enhanced and the bacterial infection waned.
The study coauthors observe that B. cenocepacia causes significant morbidity and mortality in patients with cystic fibrosis, surviving intracellularly in macrophages, and uniquely causing systemic infections in persons with CF. They note that autophagy is a physiologic process that involves engulfing non-functional organelles and proteins and delivering them for lysosomal degradation, but also plays a role in eliminating intracellular pathogens, including B. cenocepacia.
Peripheral blood monocyte derived macrophages (MDMs) were obtained from CF and non-CF donors and subsequently infected with B. cenocepacia. Basal serum levels of IFN-y were similar between CF and non-CF patients, however after B. cenocepacia infection there is deficient IFN- production in CF MDMs. IFN-y treated CF MDMs demonstrate increased co-localization with the autophagy molecule p62, increased autophagosome formation, and increased trafficking to lysosomes compared to untreated CF MDMs.
The report notes that electron microscopy confirmed IFN-y promotes double membrane vacuole formation around bacteria in CF MDMs, while only single membrane vacuoles form in untreated CF cells. Bacterial burden is significantly reduced in autophagy stimulated CF MDMs, comparable to non-CF levels. IL-1 production is decreased in CF MDMs after IFN- treatment. Together, these results demonstrate that IFN- promotes autophagy-mediated clearance of B. cenocepacia in human CF macrophages.
“The goal of the study was to show if you could stimulate autophagy, you could help clear pathogens better,” says Dr. Kopp, who also is an assistant professor of pediatrics at The Ohio State University College of Medicine. “These findings clearly suggest that is indeed the case.”
Dr. Kopp’s Laboratory at OSU researches mechanisms of disease prevention in patients with cystic fibrosis (CF). Specifically, the lab is focused on autophagy mediated clearance of pathogens such as B. cenocepacia, as well as biomarkers of new bacterial acquisition and inflammation in infants.
The study is the first in a series by Dr. Kopp and colleagues to look at autophagy mediation as a growing area of interest among clinician scientists who study CF and other disorders that affect the immune system. In CF, the need for new treatments is great. Many of the infections that plague this patient population are resistant to available drugs and some of the drugs that do work have side effects that leave many physicians unwilling to prescribe them.
“As we’re learning more about CF, were finding more and more issues with the immune system and not just the typical clearance of mucus,” Dr. Kopp says in a Nationwide Children’s release. “Now we’re discovering that there is this initial response, of which autophagy is a part, in which the immune system is not clearing the bacteria and there are some continued deficits in that in CF patients.”
According to the Centers for Disease Control and Prevention (CDC). B. cenocepacia infections have also been reported in hospitalized patients with compromised immune systems. So, Dr. Kopp added, the findings could be of interest to clinician-scientists in areas other than cystic fibrosis.
[adrotate group=”1″]
Burkholderia cepacia General Information
The CDC says Burkholderia cepacia [burkhlderuh sipaysheeuh] are a complex of bacteria commonly found in soil and water, and that B. cepacia bacteria are often resistant to common antibiotics.
Populations susceptible to B. cepacia infection
The CDC observes that B. cepacia poses little medical risk to healthy people, but that people who have certain health problems like weakened immune systems or chronic lung diseases, particularly cystic fibrosis, may be more susceptible to B. cepacia infections, and B cepacia is a known cause of infections in hospitalized patients.
Symptoms of B. cepacia infection
The effects of B. cepacia on people vary widely, ranging from no symptoms at all to serious respiratory infections, especially in patients with cystic fibrosis.
Transmission of B. cepacia infection
Transmission of B. cepacia from contaminated medicines and devices has been reported.
In 2005, CDC was notified by several states of clusters of pneumonia and other infections caused by B. cepacia and associated with contaminated mouthwash, and in 2004, CDC was notified of a voluntary recall of over-the-counter nasal spray due to contamination with B. cepacia complex. Also in 2004, B. cepacia was linked to nosocomial infections among intensive care unit patients and associated with exposure to sublingual probes.
B. cepacia can also be spread to susceptible persons by:
• Person-to-person contact
• Contact with contaminated surfaces
• Exposure to B. cepacia in the environment.
Treatment of B. cepacia infection
B. cepacia can be resistant to many common antibiotics. Decisions on the treatment of infections with B. cepacia should be made on a case-by-case basis. Careful attention to infection control procedures like hand hygiene can help reduce the risk of transmission of this organism.
Sources:
Nationwide Childrens Hospital
PLoS One
Ohio State University College of Medicine
Centers for Disease Control and Prevention