Tube Feeding Could Be Source of Drug-resistant Bacteria in CF Patients, Study Reports
Written by |
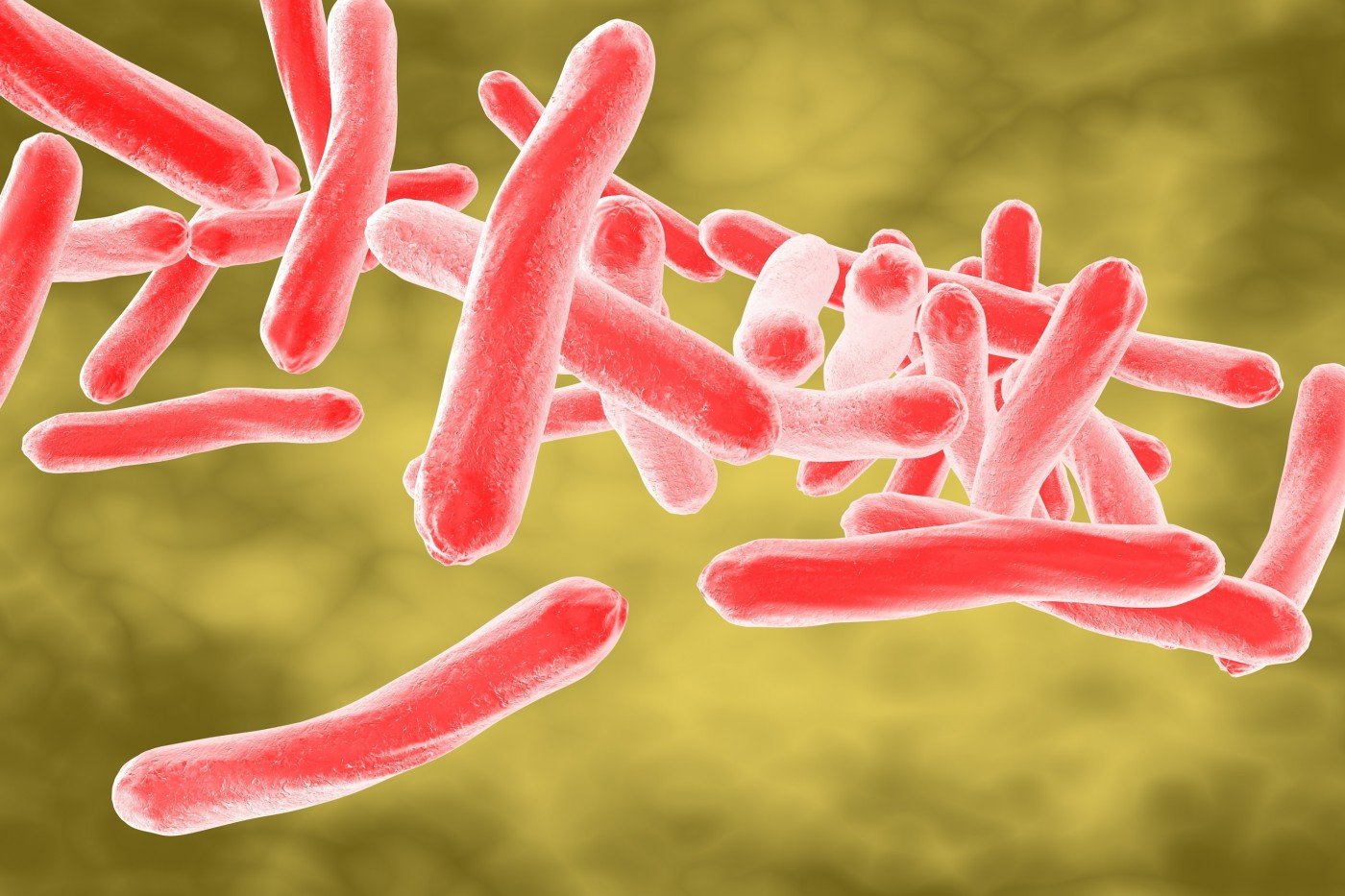
Multi-drug-resistant nontuberculous mycobacteria (NTM) can be found in the gastric juice and tubes that are used to feed some cystic fibrosis (CF) patients, research shows.
Tube feeding, known as gastrostomy, involves surgeons inserting a tube through the abdominal wall and into the stomach. Gastrostomy can also be used to drain the stomach when there’s a blockage.
The study, “Nontuberculous mycobacteria in gastrostomy fed patients with cystic fibrosis,” was published in the journal Scientific Reports.
NTM can cause many soft tissue infections. Increasingly, such infections are showing up in the lungs. NTM infection is especially worrisome in CF patients. The prevalence is as high as 32.7% of patients, depending on geographical region and patient population.
The NTM Mycobacterium abscessus complex (MABSC) is a major respiratory pathogen in CF patients. MABSC pulmonary disease in people with CF can lead to an accelerated decline in lung function and may prevent a safe lung transplant in patients with end-stage lung disease. Treatment of MABSC is not always successful and may cause adverse effects due to the multiple antibiotics that are required.
MABSC can be transmitted between CF patients despite stringent segregation. One way this can occur is through fomite contamination, or picking up bacteria through skin cells, hair, clothing or bedding in a hospital. Another way is through aerosols that CF patients generate during physiotherapy and spirometry testing.
Transmission can also occur from patients with smear-negative, culture-positive sputa, or lung fluid. This suggests that even a low level of inoculum — or material used for inoculation — could be enough for infection.
Scientists have found a gastric juice reservoir of organisms involved in CF lung infection in patients fed by a tube, a procedure whose scientific name is percutaneous endoscopic gastrostomy (PEG).
Researchers had yet to establish that there is a gastric juice culture of MABSC in CF patients, however. A British research team decided to see if there was one.
Dr. Christopher Ward of the Institutes of Cellular Medicine and Cell & Molecular Biosciences at Newcastle University Medical School in England led the research team. His group hypothesized that gastric juice and feeding devices used in PEG could be infecting CF patients with MABSC.
The researchers looked for NTM in gastric juice and sputa from 16 adults with moderate to severe CF lung disease who were being fed by a tube. They found bacteria or fungi in all gastric juice, sputa and PEG samples.
MABSC were detected in seven or 43% of patients. Scientists found the bacteria in the sputum of five of the seven.The rate of MABSC detection was higher than in previous groups studied. That could have been due to the severity of the patients’ disease or to an increased probability that tube feeding led to MABSC.
The bacteria were also detected in two of five patients whose PEG tube was removed for routine management. That would be “in keeping with the known resistance of MABSC organisms to divergent environments, including high temperature and low pH,” the team wrote.
Two patients had an identical MABSC strain in their sputum and gastric juice, suggesting a transfer of organisms from lung to stomach.
Two patients with no MABSC in their sputum did have MABSC in their gastric juice or PEG tube.
“For the first time to our knowledge, we have shown that MABSC can be isolated from the gastric juice and PEG tubes of patients with CF, in addition to sputum,” the team wrote. In addition, the team said it was the first time MABSC had been found “in a gastric sample in these patients.”
Studies of larger patient samples are needed to confirm if the stomach can constitute a reservoir of MABSC in PEG-fed CF patients, the researchers wrote. Studies also need to be done on how MABSC is transmitted because reflux and aspiration events, including coughing, can transmit infectious diseases.
Additional studies should “consider the lifelong use of antibiotics in CF patients, and their overall effect on microbiomes,” the researchers wrote.
Overall, the team concluded that gastric juice and PEG tubes may be sources of MABSC in CF patients.