Synthetic Antimicrobial Peptide Can Destroy Biofilms in CF Patients, Study Reports
A therapy that involves a synthetic cationic antimicrobial peptide (CAP) can decrease Pseudomonas aeruginosa biofilm formation alone or in combination with another antimicrobial agent called tobramycin.
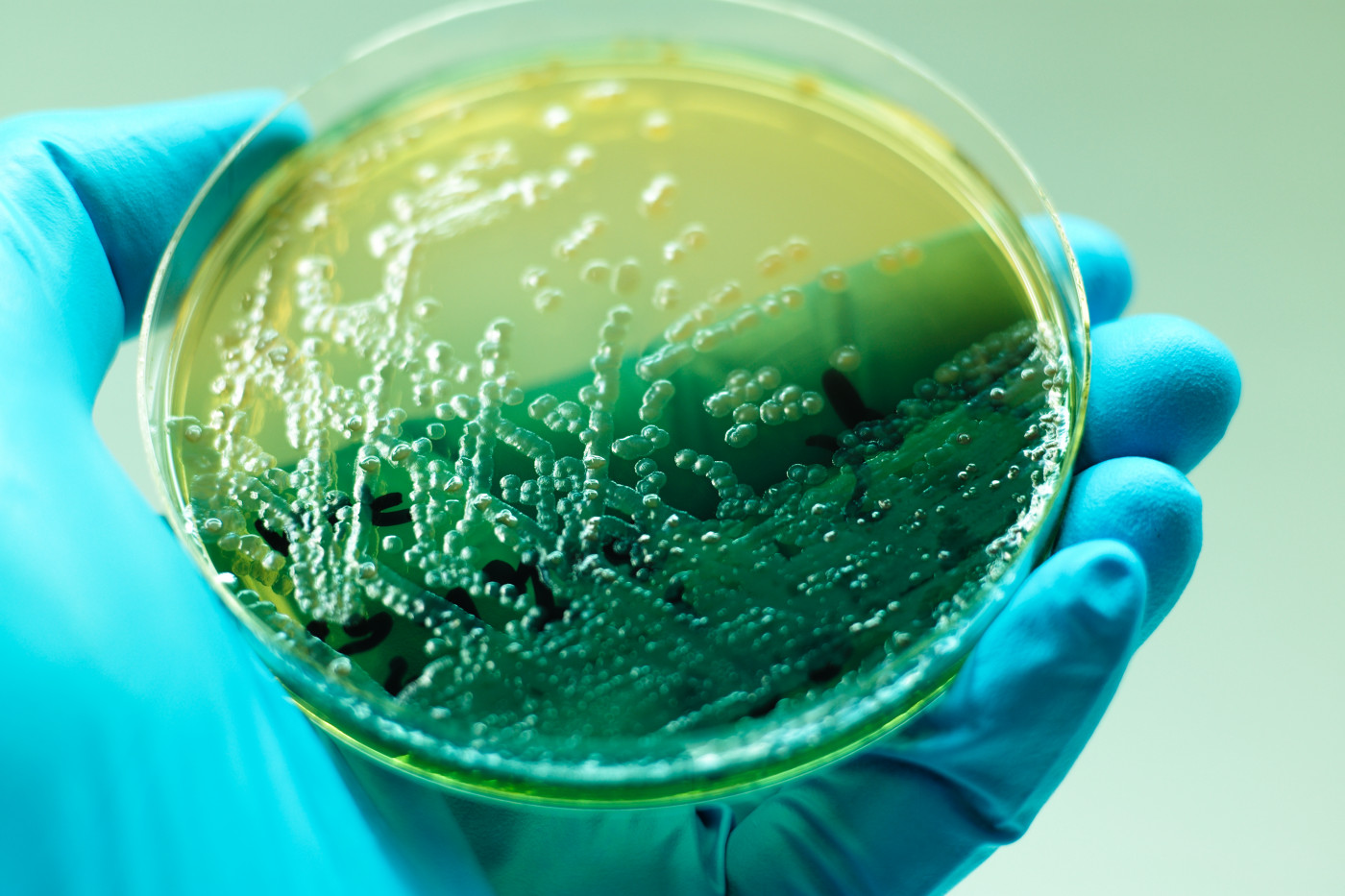
Cystic fibrosis (CF) patients are susceptible to repeated bacterial infections. Infection with Pseudomonas aeruginosa (P. aeruginosa) is particularly harmful, since it has been shown to decrease lung function and can lead to death. These bacteria, once in the lungs, can develop into biofilms — communities of bacteria that stick together and are harder to treat with standard antibiotic therapies.
Now, in the study “Activity of a novel antimicrobial peptide against Pseudomonas aeruginosa biofilms,” published in the journal Scientific Reports, a team developed a synthetic CAP and showed that it has anti-biofilm activity.
CAPs are found in a variety of organisms, and constitute a major component of the innate immune system. However, naturally occurring CAPs have adapted to their specific environments, and therefore aren’t therapeutically useful. Synthetic CAPs may overcome some of these limitations.
The team developed a synthetic CAP, called 6K-F17, with a specific sequence design that targets the bacteria but leaves the host cells alone.
Using the parental strain of P. aeruginosa, as well as several drug-resistant strains isolated from CF patients, the researchers showed that 6K-F17 can kill bacterial cells, but is not toxic toward red blood cells or cells that line the epithelium, even at high concentrations.
It is important that 6K-F17 is not toxic to cells that line the epithelium, because many antimicrobial treatments for CF patients are inhaled.
Not only could 6K-F17 kill bacterial cell isolates, but this CAP also could disrupt biofilms that had already formed. At a low concentration of 6K-F17, the biofilms lost 14% of their mass; at higher concentrations, biofilms were almost completely destroyed, leaving only 3% of the original mass.
6K-F17 could also disrupt biofilm formation from four multi-drug resistant strains isolated from CF patients, highlighting the usefulness of this new therapeutic compound.
When used in combination with a more commonly used antimicrobial, tobramycin, the effect of 6K-F17 was even greater. When used together, both drugs can be given at lower concentrations. A low dose of 6K-F17 in combination with tobramycin killed P. aeruginosa biofilms quickly and for longer periods of time.
This combination was also effective when sputum from CF patients was added to the bacterial system. Sputum contains different products that might inactivate CAPs. When used alone, neither tobramycin nor 6K-F17 could reduce biofilm mass, but when used in combination, there was a significant loss of biofilm mass even in the presence of CF sputum.
It is still critical to develop animal models to test this CAP. However, the team stated its belief in the “ultimate therapeutic utility of peptide antibiotics such as 6K-F17 in the treatment of respiratory infections.”







