Platelets Not Source of Inflammatory Markers in CF Patients’ Blood, Study Finds
Written by |
Platelets circulating in the blood of cystic fibrosis (CF) patients do not contribute to the increased levels of pro-inflammatory cytokines known to exist in these patients, and which aggravate the chronic inflammation that marks the disease, researchers reported. Their study, “Decreased TGF-β1 and VEGF Release in Cystic Fibrosis Platelets: Further Evidence for Platelet Defects in Cystic Fibrosis,” was recently published in the journal Lung.
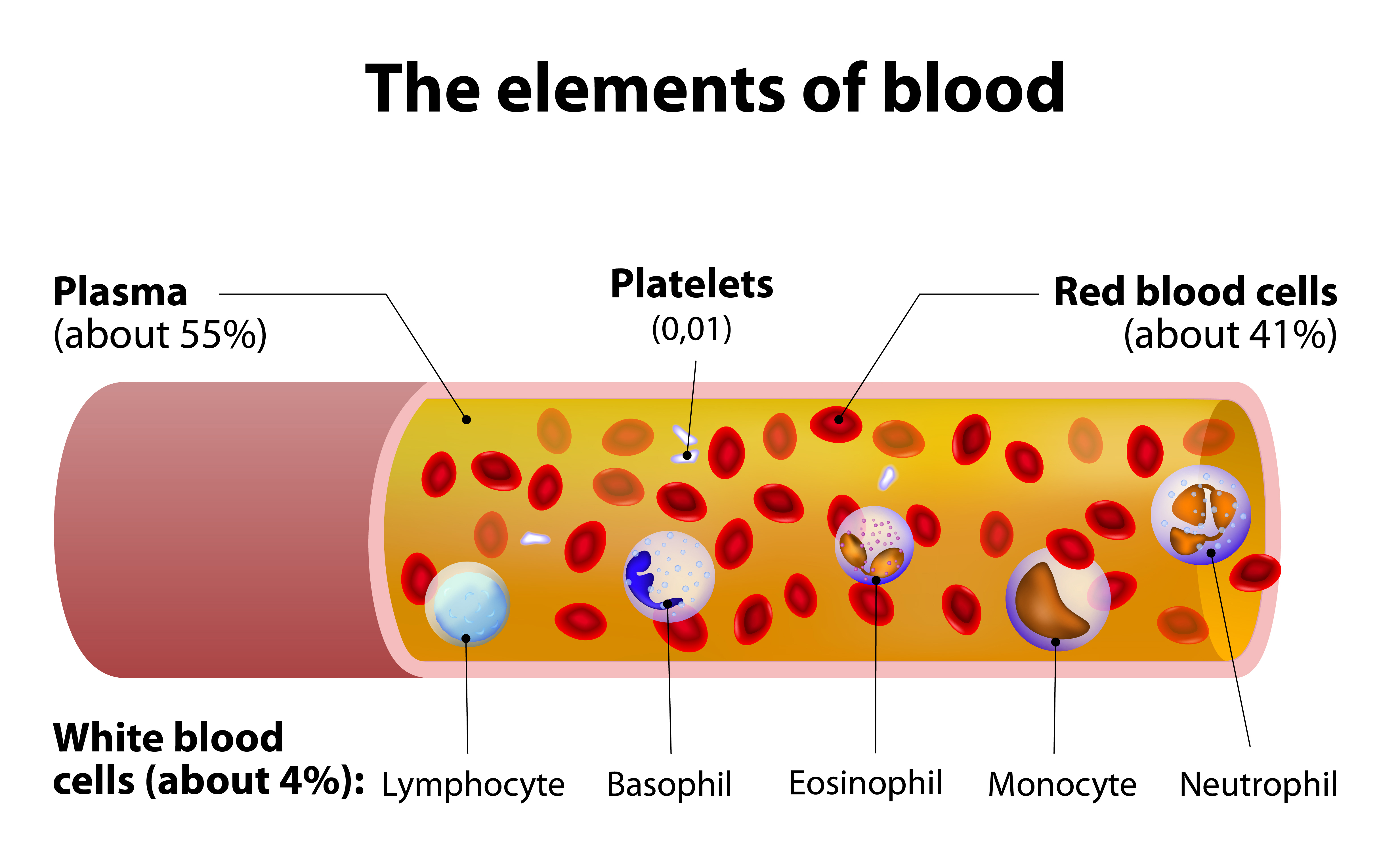
Progressive lung damage is common in patients with CF, and exacerbated by recurrent acute bacterial infections as a result of chronic inflammation. Host responses triggered by cells of the immune system, such as leukocytes (white blood cells) are also known to contribute to this process.
Platelets, another cell type present in the blood and activated by systemic inflammation, may also play an important role in worsening such inflammation. Accordingly, platelets, together with their secreted compounds, are considered potential biomarkers of disease activity and targets for therapeutic interventions. But the role of platelet-secreted cytokines in CF remains largely unknown, particularly those with inflammatory effects, such as vascular endothelial growth factor (VEGF) and transforming growth factor-β1 (TGF-β1).
A team of researchers investigated whether platelet release of the profibrotic and pro-inflammatory cytokines TGF-β1 and VEGF is altered in CF. To this end, the researchers obtained blood samples and platelets from CF patients who had recently been hospitalized or treated for an acute infection. In total, the team analyzed 21 CF outpatients and compared the results to 20 healthy controls. Both groups were measured for VEGF and TGF-β1 levels, and the information analyzed, taking into account parameters such as platelet number, cytokine release during platelet aggregation, and differences in platelet aggregation.
The investigators found that CF patients had an increased number of platelets and higher platelet aggregation levels. Additionally, the plasma and serum levels of TGF-β1 and VEGF were higher in CF patients relative to healthy controls. But after adjusting cytokine secretion to the number of platelets, there was no difference between CF patients and controls. In fact, the release of VEGF and TGF-β1 during aggregation was actually lower in platelets from CF patients compared to healthy controls (52% and 29%, respectively).
Results indicate that platelets are not a source for the increased release of the blood pro-inflammatory cytokines TGF-β1 and VEGF in CF patients. In fact, platelets from CF patients seem to secrete less of these proinflammatory/profibrotic cytokines. Additional studies are needed to fully understand the platelet secretion pattern in CF patients.






