Mucociliary Clearance, Difficult in CF, Might Be Possible by Blocking Mucus Absorption
Blocking mucus absorption in the airways through the use of certain agents can strengthen an innate airway mechanism, called mucociliary clearance (MCC), that is often impaired in lung diseases such as cystic fibrosis (CF).
The study, “Marked increases in mucociliary clearance produced by synergistic secretory agonists or inhibition of the epithelial sodium channel,” was published in the journal Scientific Reports.
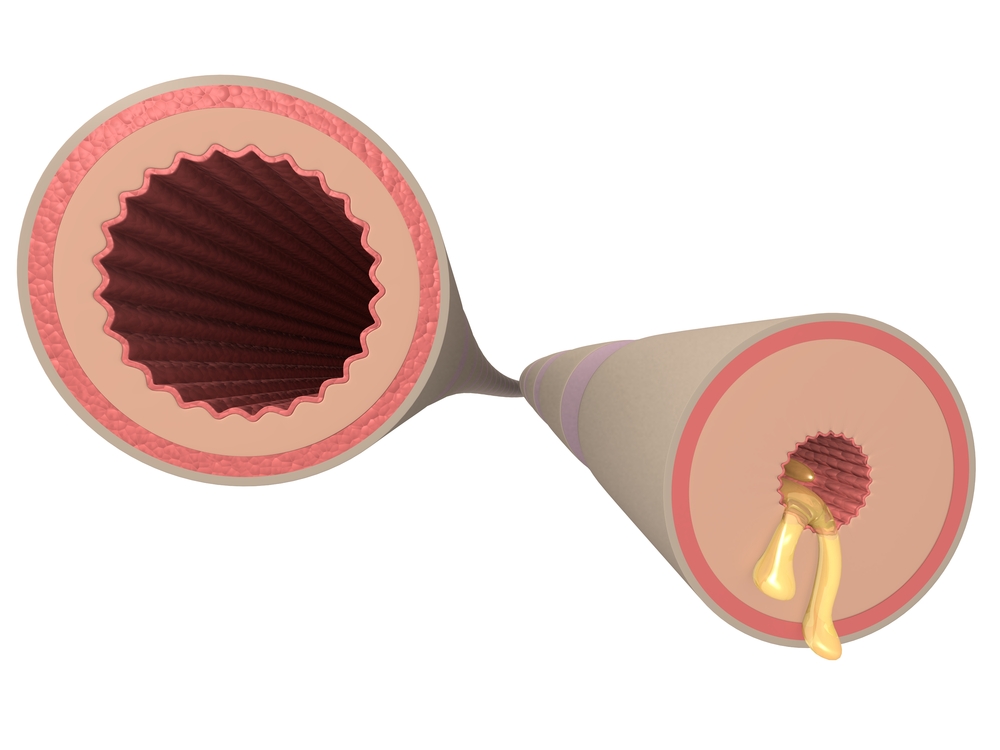
MCC is a self-cleansing mechanism by which hairlike cilia in the airways move mucus, and the trapped particulate material and pathogens it contains, out of the respiratory tract. But MCC’s efficacy depends on three major factors: the speed of ciliary beating, the properties of the mucus, and a structurally intact airway. In CF, mucus has compromised properties — it’s way too thick and sticky‚ due to by the loss of the CFTR ion channel and impaired fluid secretion.
Researchers investigated how MCC velocity might be increased. The team tested whether inhibiting fluid absorption would accelerate MCC velocity and whether blocking fluid secretion would slow it, using an ex vivo tracheal preparation (the trachea is the cartilaginous tube that connects the pharynx and larynx to the lungs).
The epithelial sodium channel (ENaC) located in epithelial cells of the lung (also found in other organs) is responsible for fluid absorption, while CFTR and calcium-activated chloride channels control fluid secretion.
Researchers found that MCC velocity was increased by agents that elevated two specific messengers, either cyclic AMP or calcium. Combining one of these messengers with an inhibitor of ENaC, called benzamil, further increased MCC velocity.
Using a CFTR-selective inhibitor, CFTRinh-172, modestly reduced the increase in MCC velocity induced by specific agents (forskolin or isoproterenol). The ENaC inhibitor, benzamil, increased MCC velocity without any boost (basal levels), and also increased velocity when used with forskolin or carbachol. Forskolin activates CFTR by raising the amount of intracellular cyclic AMP, leading to fluid secretion. Carbachol increases intracellular calcium levels.
Researchers observed that MCC velocity was particularly accelerated by the synergistic combination of forskolin and carbachol, resulting in high mucus clearance rates independent of prior treatment with CFTR or ENaC inhibitors.
These results suggest that in CF patients, whose airways are CFTR-deficient — meaning that CFTR-mediated secretion is lost — inhibiting ENaC with specific agents is a potential therapeutic strategy that may offer clinical benefits to patients.







