Pseudomonas Bacteria Infection Perpetuates Damaging Inflammation in CF Patients
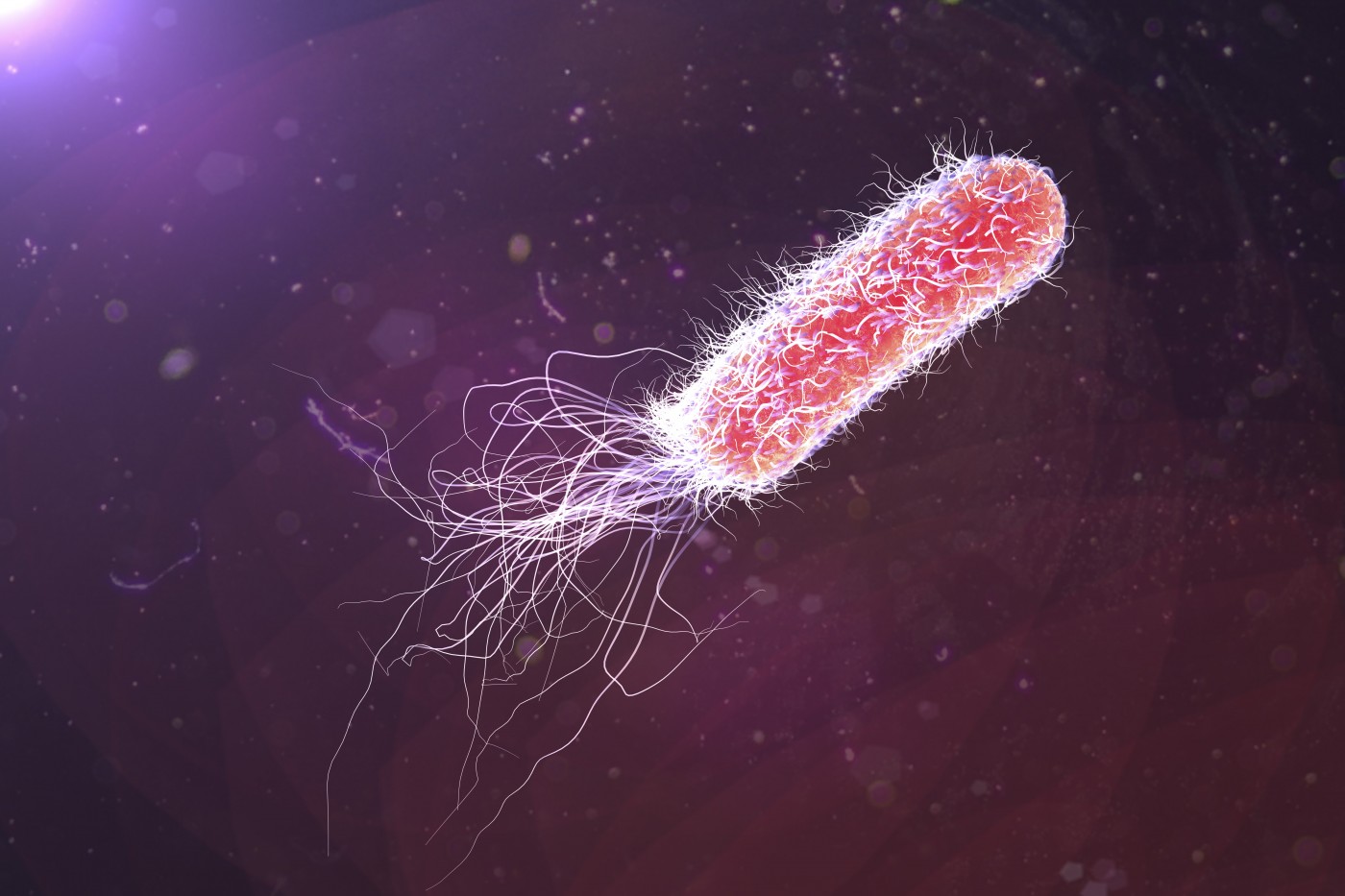
The bacteria Pseudomonas aeruginosa, which settle in the lungs of most cystic fibrosis (CF) patients, destroy the lungs by perpetuating the inflammation that aims to control invading microbes, according to a study.
This contra-intuitive finding demonstrates the power of the mechanisms bacteria use to gain a survival advantage. It also opens a new avenue of research for fighting these devastating infections.
The study, “Pseudomonas aeruginosa sabotages the generation of host proresolving lipid mediators,” was published in the journal Proceedings of the National Academy of Sciences.
Pseudomonas aeruginosa often becomes the dominant bacteria in CF patients’ lungs, thriving in a condition that stymies other bacteria — a potent inflammatory environment. In this way, they outcompete other bacteria.
Researchers are aware that the chronic inflammation damages the lungs more than the bacteria.
“Lung damage from these chronic P. aeruginosa infections, coupled with a robust but unproductive inflammatory response to the infection, will eventually lead to respiratory failure in the patient and the need for a lung transplant,” Jennifer M. Bomberger, PhD, assistant professor at the University of Pittsburgh Medical Center, said in a news release. She was a senior author of the study.
Researchers found that the bacteria maintain the inflammation by secreting a factor called Cif (cystic fibrosis transmembrane conductance regulator inhibitory factor). Cif prevents the formation of a molecule called pro-resolving lipid mediator that is crucial to resolving an inflammatory process.
Measuring the factor in lungs of children with CF, and linking their findings to medical records, the team noted that patients with more Cif in their lung mucus had weaker signaling to promote the resolution of inflammation. They also had more of the inflammatory factor IL-8 and decreased lung function.
Earlier studies indicated that increasing the level of the pro-resolving lipid mediator could harness inflammation and help get rid of the bacteria. That led to researchers believing that blocking Cif would be an even better approach.
“It will be key to devise a way to remove P. aeruginosa‘s ability to capitalize on the body’s natural inflammatory response, without eliminating that response,” Bomberger said. “Inflammation is happening for a reason — to clear infection. We just need it to temper the response when it is not effectively doing its job or is no longer needed.”







