Bone Marrow Cell Transplant May Lead to CF Treatment, Study Says
Written by |
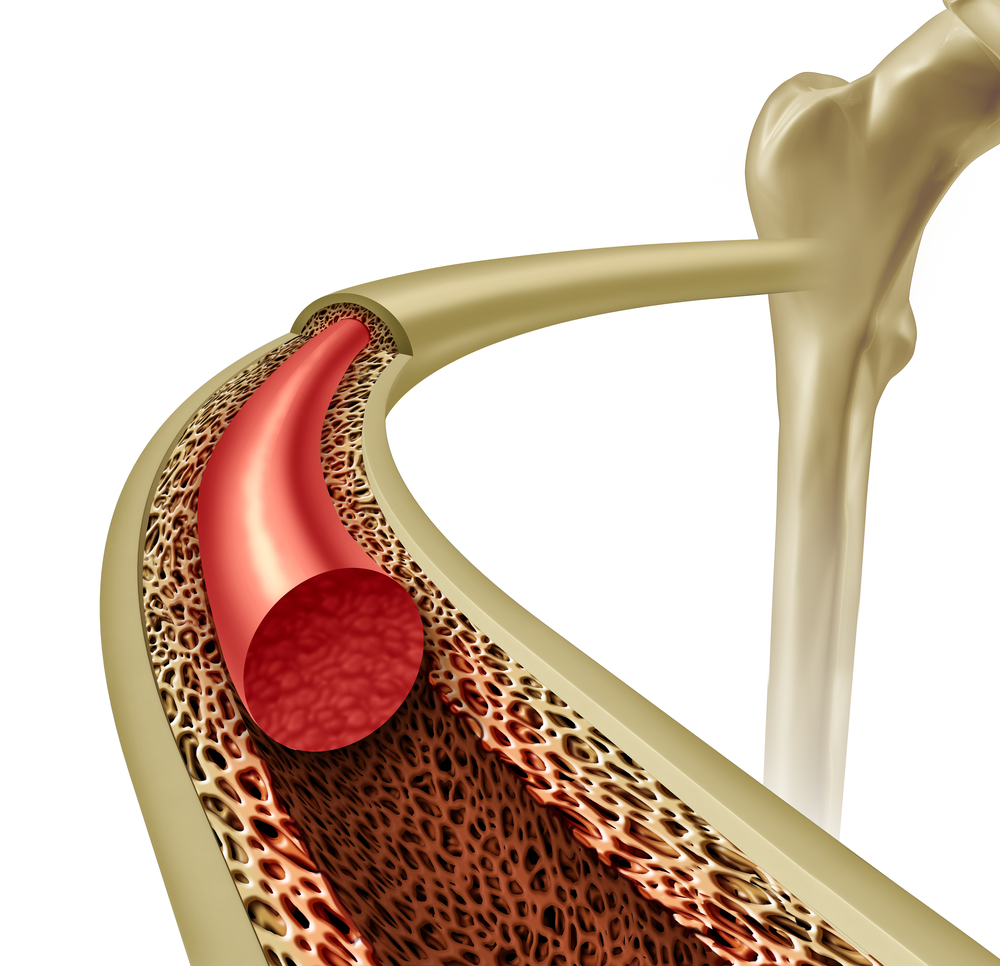
Bone marrow cell transplant can improve overall lung function and may have therapeutic benefits in treating cystic fibrosis (CF), suggests a study published in the journal Molecular Therapy.
CF is caused by a genetic mutation in the CFTR gene, leading to a defective CFTR protein. Previous research showed that cell therapy could restore production of functional CFTR protein. However, this approach has been limited due to low levels of engraftment, or incorporation of the cells.
A team of researchers led by Dr. Thomas Waddell of Latner Thoracic Surgery Research Laboratories and the McEwen Centre for Regenerative Medicine at Canada’s University of Toronto found that — using a mouse model of cystic fibrosis — an optimized delivery of normal bone marrow cells contributes to the expression of CFTR proteins in the epithelial cells of the airways and restores fatty acids, which are altered in cystic fibrosis.
The results were published in the report, “Partial Restoration of CFTR Function in cftr-Null Mice following Targeted Cell Replacement Therapy.“
Importantly, the delivery of bone marrow cells delayed lung infection with the pathogenic bacteria Pseudomonas aeruginosa and increased survival of the mice.
Researchers observed the same effects when they used bone marrow cells derived from mice with the mutated CTRF gene. But these only lasted up to six months, while the benefits of normal bone marrow cells lasted beyond six months.
Researchers concluded that bone marrow cells confer a dual benefit: an early non-specific beneficial effect against infections — possibly by recruiting macrophages and other immune cells that fight off infections — and a late beneficial effect linked to the expression of functional CTRF protein.
“We believe that CFTR expression may be restored by [bone marrow cell] delivery, resulting in long-lasting benefits in bacterial clearance and resistance to infection,” they said, while noting some potential problems associated with the clinical applications of cell replacement therapy.
Among these, for example, is the fact that the mouse model of CF does not have the thick airway mucus CF patients have. This mucus could prevent grafted cells from reaching airway epithelial cells. In addition, the body may reject the grafted cells. Researchers urge further study before translating their results to people.






