Majority of CF Patients in Small Study Treated with Antibiotics at Levels Too Low to Fight Lung Infections
Written by |
Ten of 19 cystic fibrosis (CF) patients given antibiotics to manage pulmonary exacerbations did not achieve high enough blood concentrations of the antibiotic to sustain a therapeutic effect, results of single-site study show.
This failure may be contributing to the development of antibiotic-resistant pulmonary infections, and to a worsening of pulmonary function in patients, its researchers said.
The study, “Relationship of Pulmonary Outcomes, Microbiology, and Serum Antibiotic Concentrations in Cystic Fibrosis Patients,” was published in the Journal of Pediatric Pharmacology and Therapeutics.
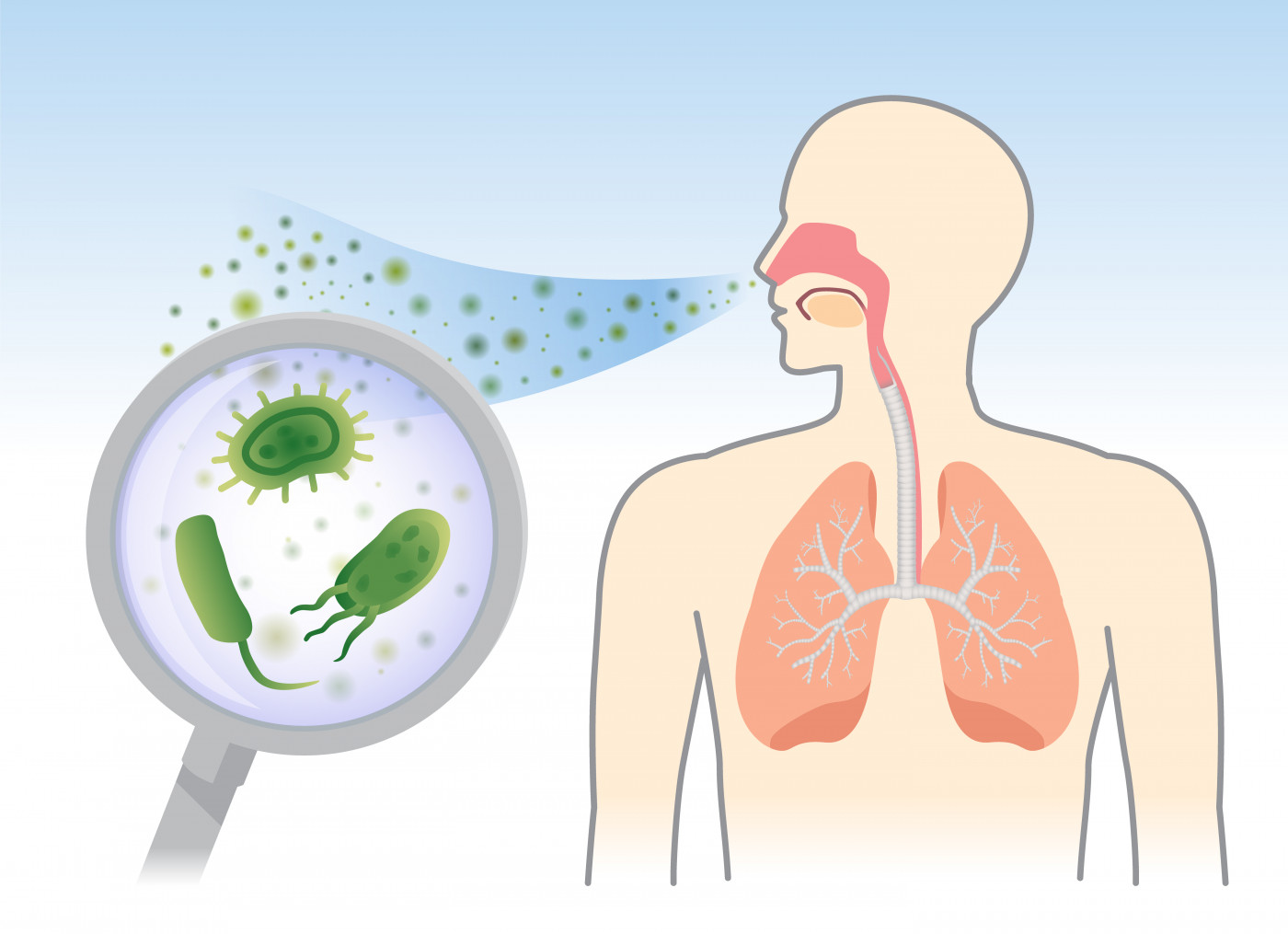
Pulmonary infections are the main reason CF patients experience acute symptom worsening, also known as pulmonary exacerbations or flares. These events are often treated with a combination of at least two antibiotics that can tackle a broad spectrum of bacteria.
Treatment regimens typically include antibiotics containing beta-lactam compounds, such as penicillin and cephalosporins. For the treatment to be effective, it is necessary to achieve a minimum antibiotic concentration in the blood for a given period of time. Reports have shown that antibiotic dosing often does not correlate with the clinical outcome in patients.
To better understand what could be contributing to poorer outcomes, researchers evaluated if CF patients reached levels of β-lactam concentrations in their blood considered therapeutically effective.
They analyzed the blood levels of broad-spectrum antibiotics based on beta-lactam compounds in 19 CF patients, ages 5 to 21, who were treated for pulmonary flares at the Children’s National Health System in Washington, D.C.
Blood samples were collected at four time points in their antibiotic treatment course — less than 30 minutes before a dose, at one hour post-infusion, three-four hours post-infusion, and less than 30 minutes before another dose is infused.
All patients underwent pulmonary function tests.
Based on pre-established values of minimum concentrations needed to inhibit each pathogen, and the antibiotics’ previously reported stability, the team determined therapeutic and sub-therapeutic antibiotic exposure.
During roughly one year, the 19 patients received a total of 29 courses of antibiotics. The most common β-lactam antibiotics used were ceftazidime (62%; sold under the brand names Fortaz and Tazicef, among others), and Merrem (45%; meropenem).
Analysis revealed that 47%, or nine patients, reached therapeutic blood levels of the antibiotics tested; the other 10, or 53%, did not. Evaluation also showed no significant differences in age, CF-associated genetic mutation, or kidney function between the optimal and sub-optimal patient groups.
Those with optimal antibiotic concentrations had better responses on the spirometry tests, indicative of better pulmonary function.
“We found that sufficient antibiotic exposure during treatment of CF pulmonary exacerbations was associated with improved pulmonary function,” the researchers wrote.
However, researchers were unable to predict which patients would achieve therapeutic antibiotic concentration based only on information about the antibiotic dosing regimen used.
“This suggests that CF patients may benefit from closer monitoring of their beta-lactam exposure and bacterial MIC [minimum inhibitory concentration] for optimal clinical outcomes,” they wrote.
The team is currently evaluating if real-time monitoring of antibiotic blood concentrations could help clinicians in determining whether a CF patient is receiving enough antibiotics to fight a pulmonary infection.
“Getting adequate treatment is crucial for getting better,” Andrea Hahn, MD, MS, an infectious disease specialist at Children’s National and lead author of the study, said in a news release.






