Large Sugar Molecule Disrupts B. cepacia Bacteria from CF Patients, Study Shows
Written by |
An experimental large sugar molecule called poly (acetyl, arginyl) glucosamine, or PAAG, was able to disrupt treatment-resistant biofilms formed by Burkholderia cepacia complex bacteria extracted from patients with cystic fibrosis (CF), according to a study.
The study, “In Vitro Activity of a Novel Glycopolymer against Biofilms of Burkholderia cepacia Complex Cystic Fibrosis Clinical Isolates,” was published in the journal Antimicrobial Agents and Chemotherapy.
Burkholderia cepacia complex (Bcc) is a strain of opportunistic bacteria that can cause lower respiratory infections in patients with CF. They often appear late in CF progression and form biofilms (layers of bacteria sticking to surfaces or each other) that impede the penetration of antibiotics, reducing their therapeutic effects.
Combination therapies using different antibiotics are a common approach to eradicate bacteria from the lungs. However, the failure to eliminate the colonies from the lungs of CF patients has contributed to the development of antibiotic-resistant bacteria.
Researchers from Synedgen and their collaborators decided to test a new experimental treatment strategy based on using PAAG, a complex large sugar molecule belonging to a class known as glycopolymers. Previous treatment with PAAG on different strains of bacteria demonstrated its antibacterial activity and ability to increase permeability and decrease resistance.
Ask questions and share your knowledge of Cystic Fibrosis in our forums.
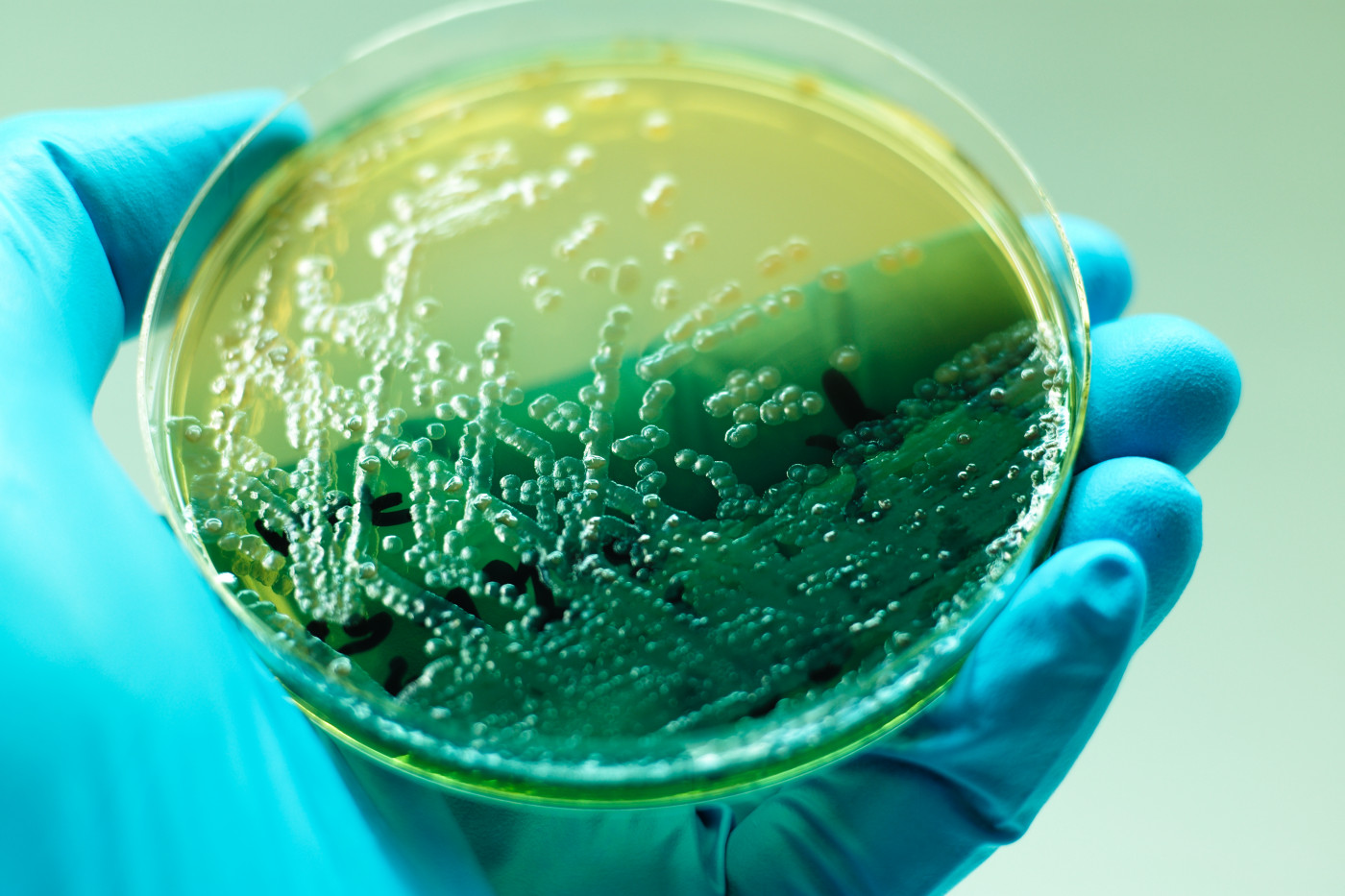
The team evaluated the ability of PAAG to disrupt Bcc biofilms formed by different Burkholderia cepacia isolates collected from CF patients as well as to decrease the number of live bacteria in vitro, or in culture in the laboratory.
They used 13 Burkholderia cepacia isolates from 11 CF patients (age ranging between 13 and 34 years) that included different bacteria species, such as B. multivorans, B. cenocepacia, B. gladioli, B. vietnamiensis, B. dolosa, and B. cepacia. Most of the isolates were resistant to three commonly used antibiotics: Merrem (meropenem, 69% resistant isolates), tobramycin (69% resistant), and ceftazidime (53% resistant).
To assess differences in biofilm mass or live bacteria upon PAAG treatment, the researchers counted and visualized bacterial growth by measuring the sample density through light absorbance and using microscopy, respectively.
PAAG significantly reduced Bcc biofilm masses in a dose- and time-dependent manner. Biofilm mass was reduced 15- to 20-fold after just 10 minutes of treatment with the highest tested PAAG amount (200 mcg/mL), and 25-fold one hour after treatment, compared with non-PAAG-treated bacteria cultures.
Effects of PAAG were also found to be dependent on the specific isolates tested, establishing the most robust reduction in B. cenocepacia out of all the tested isolates.
Treatment with PAAG also induced a reduction of biofilm thickness by approximately 75–80% on all tested bacterial species compared with those treated with inactive or control compounds. The observed decrease in thickness was found on mature biofilms that had been grown for a longer period of time (48 hours), using both lower and higher PAAG concentrations (100 and 200 mcg/mL).
As a complement to the biofilm mass measurement, the researchers also assessed the number of remaining live bacteria after biofilm disruption with PAAG treatment. Again, they saw a significant and dose-dependent reduction in live bacteria one hour after treatment, while treatment with inactive controls resulted in no significant changes.
“PAAG was able to significantly facilitate disruption and removal of preformed biofilms from all six Burkholderia clinical species frequently associated with CF lung infections,” the researchers said.
They also noted that the biofilm disruption occurred early after treatment (10 minutes), which they suggested could be translated into effective and short therapeutic treatment times. Still, according to them, these types of in vitro analyses may not represent the complexities of the CF condition and will require more studies.
“Rapid disruption of mature Bcc biofilms’ cohesion by PAAG supports its use in combination with standard-of-care antibiotics during treatment of identified infection or exacerbations,” they said. “Development of PAAG for clinical use has the potential to significantly improve treatment of recalcitrant Bcc biofilm infections associated with CF and to potentiate the activity of antibiotics.”






