Aerosolized Therapy Restores CFTR in Patient-derived Cells
ReCode Therapeutics’ investigational aerosolized RNA-based therapies for cystic fibrosis (CF) restored CFTR function, the defective protein in CF, in patient-derived lung cells.
Delivered by the company’s selective organ targeting (SORT) lipid nanoparticle (LNP) platform, the therapy showed no signs of toxicity in epithelial cells that line the airways.
“Today’s presentation confirms that our SORT LNP platform can deliver optimized, functional CFTR mRNA as an aerosol to the intended secretory and basal cells in the airway epithelium,” David Lockhart, PhD, chief scientific officer and president of ReCode, said in a press release.
The data were presented at the American Thoracic Society International Conference 2022, May 13–18, as a poster titled, “Functional Rescue of CFTR by Aerosolized Delivery of Optimized CFTR mRNA Using ReCode LNPs in Primary Human Bronchial Epithelial Cells Derived From Patients With Cystic Fibrosis.”
In CF, variants of the CFTR gene lead to defects in the encoded CFTR protein, which functions as a chloride channel that helps regulate the movement of water in tissues. When the CFTR protein is impaired, mucus that lines the airways thickens, leading to recurrent infections, inflammation, and other symptoms.
CFTR modulators are a specialized group of therapies designed to address specific defects in the CFTR protein. However, about 10% of people with CF are not amenable to these therapies. That’s why treatments that promote CFTR function and mucus clearance are still needed.
ReCode is developing a treatment to rescue CFTR function using messenger RNA (mRNA) — the molecule that carries the genetic instructions to make protein.
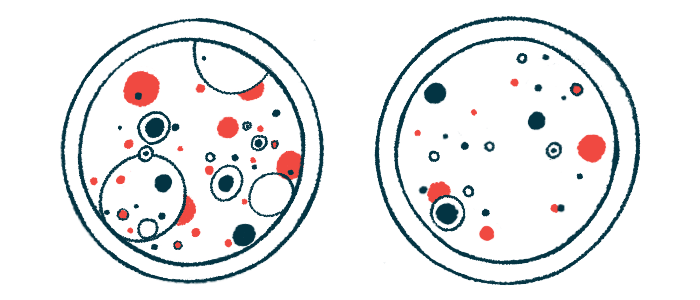
The inhaled therapy uses the company’s first-in-class SORT LNP delivery platform, which aims to bring CFTR mRNA into the lungs to facilitate the production of healthy CFTR protein. LNPs are fat-like bubbles containing the mRNA that fuse with cell membranes.
Scientists at ReCode, the Rosalind Franklin University of Medicine and Science in Illinois, and the University of Texas Southwestern Medical Center, conducted a series of cell-based experiments as a proof of concept to demonstrate the preliminary effectiveness of this new therapeutic.
Because naturally occurring CFTR mRNA is subject to degradation, nucleotides — the building blocks of mRNA — first were modified to ensure stability.
Epithelial cells from rats were used to evaluate different CFTR mRNA candidates. CFTR function tests, measuring the flow of chloride, distinguished modified candidates that significantly enhanced protein function beyond that of naturally occurring CFTR mRNA.
Next, epithelial cells from the lung’s bronchial tubes (hBE) — derived from a CF patient that carried CFTR gene mutations — were grown (differentiated) at an air-liquid interface. Cells then then aerosolized with different LNP formulations containing the lead CFTR mRNA candidate. One LNP formulation, referred to as LNP A, showed the highest enhancement of CFTR activity.
The same hBE cells then were exposed to low, medium, and high doses of LNP A, demonstrating an increase in CFTR function in a dose-dependent manner. Moreover, the team measured the levels of LDH in the surrounding fluid, a secreted biomarker for cell toxicity. Even at the highest dose, they detected no toxicity.
hBE cells with multiple different CFTR gene mutations (genotypes), some of which responded to the CFTR modulator therapy Trifakta and others that did not, were exposed to the high-dose LNP A aerosol treatment. Across all cells, regardless of the underlying mutation, CFTR protein function was restored.
Finally, four main types of healthy lung epithelial cells, including ciliated, club, goblet, and basal cells, were exposed to the lead CFTR mRNA molecule modified with a fluorescent tag, which allows the medicine to be visualized under a microscope. The therapy was internalized within all cell types, with the highest levels in goblet cells that secrete mucus.
“In human bronchial epithelial cells derived from CF patients, we have shown that delivery of our CFTR mRNA results in consistent rescue of CFTR function with multiple genotypes, including those types that account for approximately ten percent of the CF population who do not respond to currently approved CFTR modulators,” Lockhart said. “We are eager to continue development of this promising therapy.”








