New Research Into Bacterial Behavior Could Aid in Mitigating Antibiotic Resistance in CF Patients
Written by |
Researchers from The University of Texas at Austin recently revealed that the pathogenic bacteria Pseudomonas aeruginosa has the capacity to inhibit its own growth and the growth of antibiotic-resistant mutants. The study entitled “The spatial profiles and metabolic capabilities of microbial populations impact the growth of antibiotic-resistant mutants” was published in the Journal of the Royal Society Interface by Karishma Kaushik, and Vernita Gordon, senior author, from the University of Texas at Austin, along with colleagues. The results could have implications in addressing antibiotic resistance in cystic fibrosis patients.
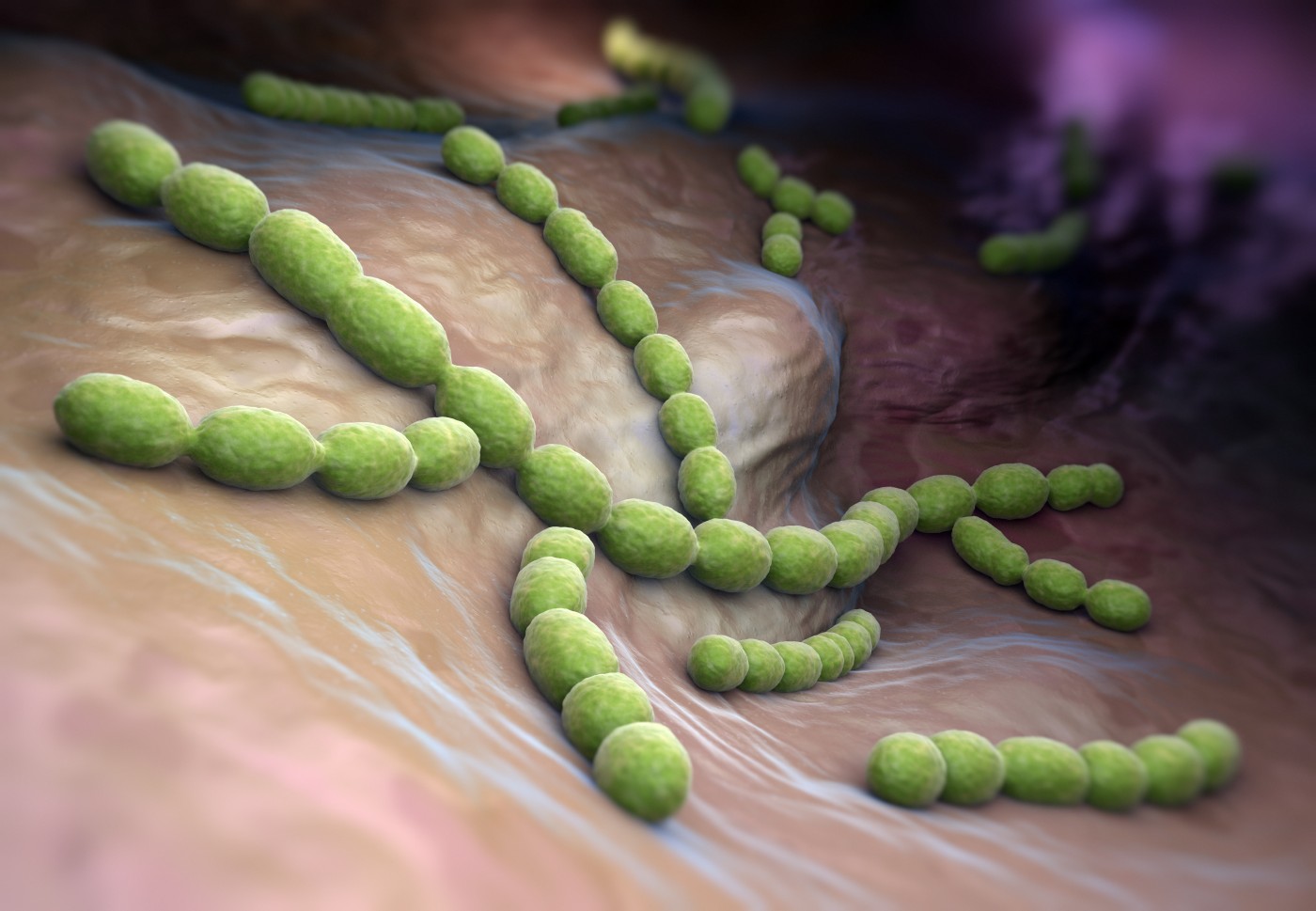
Pseudomonas aeruginosa (P. aeruginosa) are bacteria that normally cause pneumonia in hospital patients and deadly infections for cystic fibrosis patients, individuals with HIV and chronic wounds. P. aeruginosa belongs to a class of pathogenic bacteria that are starting to become progressively antibiotic-resistant, which includes E. coli, the main cause of urinary tract infections, and N. gonorrhoeae, which causes gonorrhea.
“This means we can start to think about the population of microbes as another set of knobs you could turn to fight infection,” said Vernita Gordon in the news release.
The research team found that the P. aeruginosa bacteria produce a by-product that has the ability to change the pH balance that inhibits the development of antibiotic-resistant bacteria among them. This result reinforces the idea that by adding a base — a compound with higher pH — to some inhaled therapies together with antibiotics, it could help to fight these bacteria, for example in cystic fibrosis patients. This strategy would decrease antibiotic resistance and at the same time allow clinicians to decrease antibiotic dosages for toxic antibiotics when given at high doses that often lead to adverse side effects such as deafness and kidney damage.
Prof. Bryan Davies from the Center for Infectious Disease at the University of Texas said this study suggests that for some type of infections the design of the antibiotic formulation should promote the generation of a basic environment in the infection site to obtain a more efficacious treatment.
These findings may contribute to the development of improved strategies to combat a class of bacteria that has become increasingly resistant to antibiotic therapies. The study was financially supported by ExxonMobil, The University of Texas and the Department of Physics of the university at Austin.






