CF bacterial infections usually persist after Trikafta is started
P. aeruginosa still detectable in 18 of 19 adults who started treatment
Infections of Pseudomonas aeruginosa usually persist in people with cystic fibrosis (CF) after Trikafta is started, a study reports.
The study, “Persistence and evolution of Pseudomonas aeruginosa following initiation of highly effective modulator therapy in cystic fibrosis,” was published in mBio.
CF is caused by mutations in the gene that encodes the CFTR protein. Without a functional version of it, the body produces abnormally thick and sticky mucus. In the lungs, this mucus provides a fertile breeding ground for bacteria and chronic lung infections are a major issue in CF. P. aeruginosa is one of the main types of bacteria that causes problematic lung infections in CF patients.
Trikafta is a triple-combination therapy that contains elexacaftor, tezacaftor, and ivacaftor to increase the functionality of the defective CFTR protein in people with CF caused by specific mutations. In the U.S., it’s approved for eligible patients as young as 2.
Trikafta can help normalize mucus production and improve lung function, but its effects on chronic bacterial infections aren’t fully understood.
Changes in P. aeruginosa levels, and mutations
Here, scientists analyzed samples from the airways of 19 adults with CF who had chronic P. aeruginosa infections and started Trikafta. The total number of bacteria tended to decrease after the patients started treatment, but P. aeruginosa was still detectable in 18 of them.
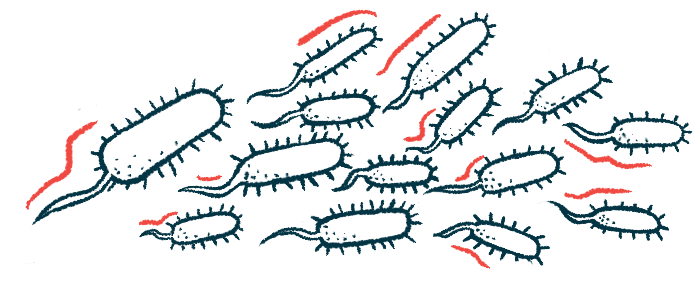
“P. aeruginosa persists in the respiratory tract post-[Trikafta] in virtually the entire cohort,” wrote the researchers, who also performed genetic analyses of the bacterial samples, which confirmed that the strains of P. aeruginosa found after starting Trikafta were largely the same ones that had been there before the therapy was started, though in some cases new strains were seen.
The P. aeruginosa bacteria sampled after Trikafta was started carried mutations that hadn’t been there before. This finding in itself isn’t that surprising, since bacteria will always acquire new mutations over time, but the number of new mutations in these P. aeruginosa samples post-Trikafta was strikingly higher than what would be expected in bacteria from untreated patients.
This is likely because Trikafta is working as expected, said the researchers. Bacteria living in the airways face a sudden and dramatic shift in their environment. As a result, many bacteria die and those that survive are faced with new evolutionary pressures, which leads to shifts in the population’s genetic makeup.
“We found that P. aeruginosa undergoes a population bottleneck coincident with the initiation of [Trikafta], followed by drastic changes to the mutational spectra of the P. aeruginosa population due to new selective pressures in the post-[Trikafta] airway environment. This bottleneck is likely explained by changes in the CF respiratory environment caused by corrected CFTR function,” said the scientists, who noted the clinical consequences of this continued bacterial evolution aren’t yet clear.
Still, the findings show that P. aeruginosa infections may still pose health risks for people on Trikafta and, for this reason, “the role and potentially changing face of infection in CF should not be discounted in the era of [Trikafta],” they said.