CF Researchers Identify Signaling Networks Controlling Mutant CFTR Protein Folding
Written by |
A new study published in the journal e-LIFE has taken a novel approach to looking at deficits in protein folding associated with mutations in the CF transmembrane conductance regulator (CFTR) gene, the underlying cause of cystic fibrosis (CF). By identifying the signaling networks controlling protein folding, the study opens up new possibilities for drug development.
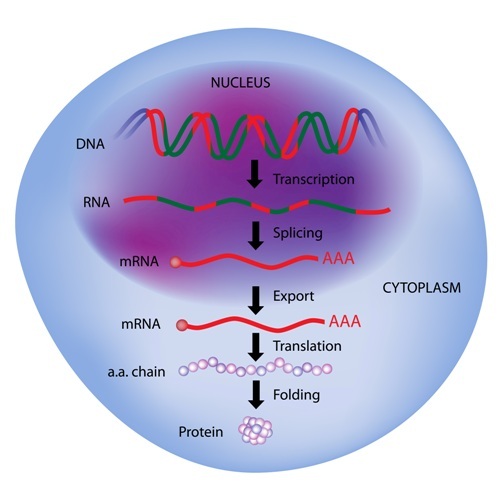
The most common mutation in the CFTR gene in CF patients is a single lacking amino acid — a phenylalanine at position 508. While this change might seem small, the cellular machinery folding a chain of amino acids into a functional protein recognizes the protein as flawed and sends it for destruction. The new study, titled “Unravelling druggable signaling networks that control F508del-CFTR proteostasis,” could be a major step forward in the understanding of mechanisms controlling the degradation of mutant CFTR.
The process of protein production, folding, and degradation, known as proteostasis, has been extensively studied in CF. How the process is controlled by cellular regulatory signaling networks, however, is less clear. Such pathways — composed of kinases, GTPases, and second messenger molecules that regulate processes by adding and removing phosphates and other chemical moieties — are known to regulate most cellular activities.
Several drugs have been identified that are able to rescue a misfolded CFTR protein from destruction. Such drugs, known as proteostasis correctors, are of clinical interest since a misfolded CFTR protein reaching the cell membrane can be functional, although working at a lower rate. These partly functional proteins contribute to decreasing symptoms, but so far, they have not reached clinical trials.
Realizing that current CFTR proteostasis correctors do not share a common and known mechanism of action, study author Ramanath Narayana Hegde and colleagues from the Institute of Protein Biochemistry in Naples, Italy, instead decided to look at potential corrector mechanisms among the side effects of these drugs.
The study, which was performed in collaboration with several other Italian institutions and McGill University, Canada, used an ambitious approach, combining experimental studies with bioinformatics to unravel factors regulating CFTR degradation.
By looking at gene expression profiles following treatment with different correctors, the team could see which genes were altered in the same way when exposed to different drugs. To expand the search, the team looked both at cultured cells and gene expression databases.
Using results from the gene expression screening, it then analyzed the role of the genes to identify pathways involved in the regulation of protein folding. The team identified and validated a number of pathways — including MAP kinase cascades — involved in the correction mechanisms of the investigated drugs.
It also found signaling networks that, if stimulated, hindered the correction of misfolded CFTR. And it observed that in cells exposed to pro-inflammatory factors, such as TNFα or oxidative stress, the degradation of the mutant proteins was further increased.
These findings might indicate that the inflammation often present in the lungs of CF patients is triggering a negative spiral of events, leading to increased CFTR protein degradation, which in turn leads to more inflammation and fibrosis.
Using the genes identified in the first round of experiments, the team next turned to a database of kinase activity to identify drugs with more potent and selective corrector activity. An advantage of this approach is that a large part of drugs already on the market or currently in clinical trials are acting on kinase signaling pathways. The activity of many factors in these pathways are also easily modified by drugs.
Another key finding was that when the team used corrector drugs in combination with a pharmacochaperone — a pharmaceutical that can rescue folding of misfolded proteins — the effects were dramatically better than when correctors or the pharmacochaperone was used separately.
The study hence demonstrates new possibilities for drug development in CF, targeting CFTR protein folding.






