Study Shows Value of Biofilm Component in P. aeruginosa Resistance
Written by |
Differences in Psl, a complex sugar molecule produced by Pseudomonas aeruginosa, contribute to the bacterium’s resistance against the antibiotic tobramycin in children with cystic fibrosis (CF), a study shows.
While tobramycin-resistant P. aeruginosa produced similar levels of Psl to those that were effectively eradicated with the antibiotic, its Psl molecules exhibited different binding profiles that affected the bacterium’s ability to aggregate and resist tobramycin.
However, since these results were based on bacteria collected from children with CF and grown in the lab, similar analyses directly in the sputum of these children are needed to confirm the findings.
Also, further studies are needed to clarify the causes of Psl’s binding differences and how these differences affect P. aeruginosa aggregation.
The study, “The role of Psl in the failure to eradicate Pseudomonas aeruginosa biofilms in children with cystic fibrosis,” was published in the journal npj Biofilms and Microbiomes.
The characteristic accumulation of thick mucus in CF patients’ lungs increases their vulnerability to respiratory infections, with the most common being those caused by the opportunistic bacterium P. aeruginosa.
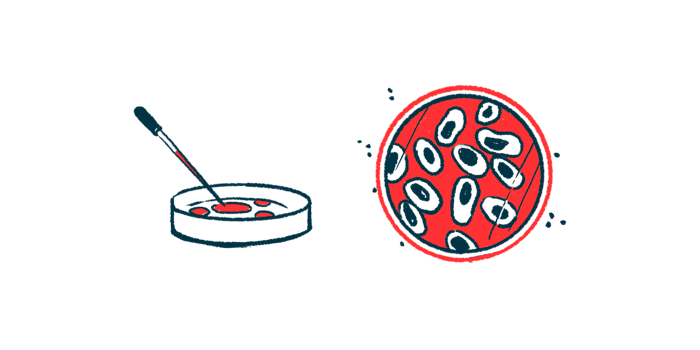
Its ability to produce biofilms — slimy layers of microorganisms that stick to wet surfaces and other bacteria — can protect the bacteria from the host’s immune response and from antibiotics.
Increasing evidence suggests that Psl, a key component of the bacterium biofilms, is involved in these mechanisms of resistance, but “its contribution to the persistence of P. aeruginosa in the CF airways following inhaled antibiotic treatment is not known,” the researchers wrote.
To address this, researchers in Canada, the U.S., and at AstraZeneca, investigated whether there were any differences in Psl between P. aeruginosa that were successfully eradicated and those that persisted with tobramycin, an inhaled antibiotic, in children with CF.
They used sputum samples from 67 pediatric CF patients undergoing eradication tobramycin treatment at the Hospital for Sick Children (SickKids), in Canada, and oropharyngeal swab samples from 14 children with CF who participated in a previous Phase 2 trial called EPIC (NCT00097773).
They first compared the amount of Psl produced by eradicated and persistent P. aeruginosa collected from the SickKids group samples. After allowing the bacteria to form biofilms in lab dishes, three antibodies that recognize distinct parts of the sugar molecule were used to quantify Psl.
Results showed no significant differences in Psl levels between the 63 samples of P. aeruginosa successfully eradicated with tobramycin, and the 29 samples of resistant bacterium.
However, Psl0096, one of the three anti-Psl antibodies, was found to bind significantly more to biofilms of persistent versus eradicated P. aeruginosa from both SickKids and EPIC patients.
“It is possible that persistent isolates grown as biofilms produce more surface Psl with a conformation that allows Psl0096 to bind more avidly than do eradicated isolates,” the researchers wrote.
Psl0096 binding in persistent P. aeruginosa was associated with greater aggregation, as well as greater tolerance to high doses of tobramycin in lab-grown biofilms, compared with eradicated P. aeruginosa.
Further analysis showed no significant differences in the number of genetic changes in Psl genes between resistant and cleared bacteria that could explain these binding differences.
Also, while the bacterial aggregation may have been caused by interactions between Psl0096 and P. aeruginosa cells, this potential mechanism did not appear to involve CdrA, a Psl-associated protein that promotes bacterial aggregation.
Notably, patients with such invasive infections are known to produce antibodies against Psl, but it remains unclear “whether anti-Psl antibodies can be detected in the sputum of CF patients colonized with P. aeruginosa,” the team wrote.
Overall, these findings suggest that “differences in Psl are important in the persistence of P. aeruginosa infection in most children with CF,” the researchers wrote, adding that this biofilm component “represents a potential therapeutic target to improve P. aeruginosa eradication treatment.”
Still, future studies, including those directly analyzing the sputum of CF pediatric patients, are needed to confirm these results and to clarify the causes and effects of these binding differences, the team noted.