Antibiotic Resistance in Cystic Fibrosis Patients Explored Using Whole Genome Sequencing
In a recent study entitled “Comparative genomics of non-pseudomonal bacterial species colonising paediatric cystic fibrosis patients,” researchers performed a whole-genome profiling of bacterial strains, that are not Pseudomonas aeruginosa, from pediatric cystic fibrosis patients and determined their link to antibiotic resistance. The study was published in the open access publisher PeerJ.
Cystic Fibrosis (CF), a life-threatening disease affecting approximately 70,000 people worldwide, is characterized by progressive lung function decline. The disease is caused by mutations in the Cftr gene (cystic fibrosis transmembrane conductance regulator gene). The CFTR protein is responsible for trafficking chloride and sodium ions in and out of cells of lungs and intestinal epithelium, and so in the absence of CFTR functional protein, thick mucus accumulates, making CF patients more susceptible to infections.
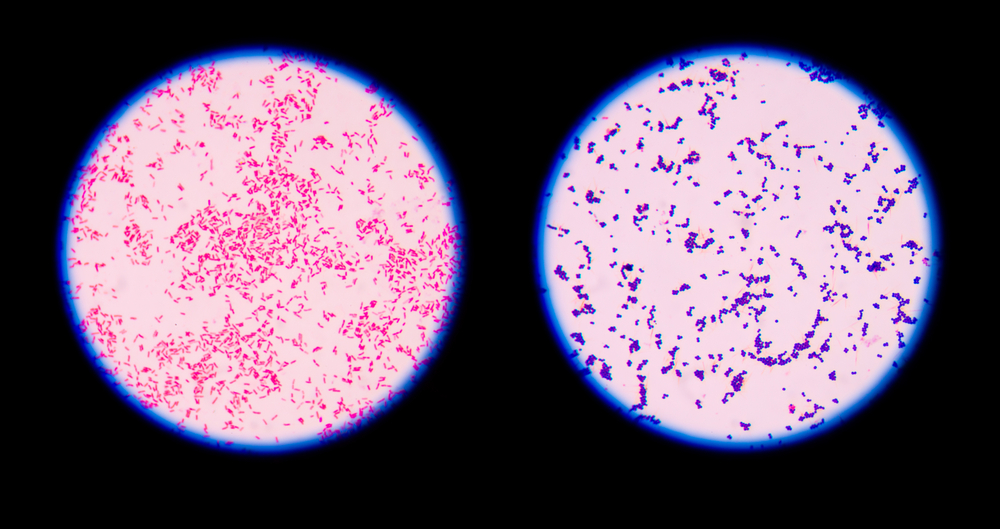
Pseudomonas aeruginosa is the most common organism causing lung infections in CF patients and targeted therapies against this strain of bacteria have significantly improved patients’ outcomes. However, removing the fittest pathogen may allow the proliferation of other microorganisms, particularly those that carry antibiotic-resistance (due to the long-term antibiotic therapy CF patients are submitted to).
In this new study, authors profiled 28 bacterial strains (that are not Pseudomonas aeruginosa) isolated from three children with CF using whole-genome sequencing to detect if indeed there were indicators for antibiotic resistance or unique virulence traits. The team did not find any evidence for increased antibiotic resistance in these isolates, neither for alterations to isolates’ gene virulence profiles, when compared to other isolates of the same species. The team notes, however, that they did not have access to patients’ health conditions and could not correlate these isolates with decline in lung function or disease exacerbations.
RELATED: Genetic Background May Determine Disease Severity in Cystic Fibrosis
The team detected that two bacteria strains – Staphylococcus aureus and Achromobacter xylosoxidans – resistant even in the presence of appropriate antibiotic therapy, which suggests that the antibiotic treatment may not reach susceptible populations of bacteria. Possible mechanisms responsible for this phenotype are the existence of physical barriers and inactivation of antibiotics action. The multi-drug resistant Achromobacter xylosoxidans was capable of persisting for almost five years, while the same was not observed for another isolated multi-drug resistant strain, the Stenotrophomonas maltophilia.
Altogether, the authors noted that their findings identified non-pseudomonal bacteria species in CF patients and particular attention should be given to Achromobacter xylosoxidans, since it can persist for long periods of time, possibly by mediating antibody resistance.







