#ECFS2018 – Multiple Sclerosis Therapy Boosts Antibiotic’s Ability to Kill Resistant P. aeruginosa Strains, Study Finds
Written by |
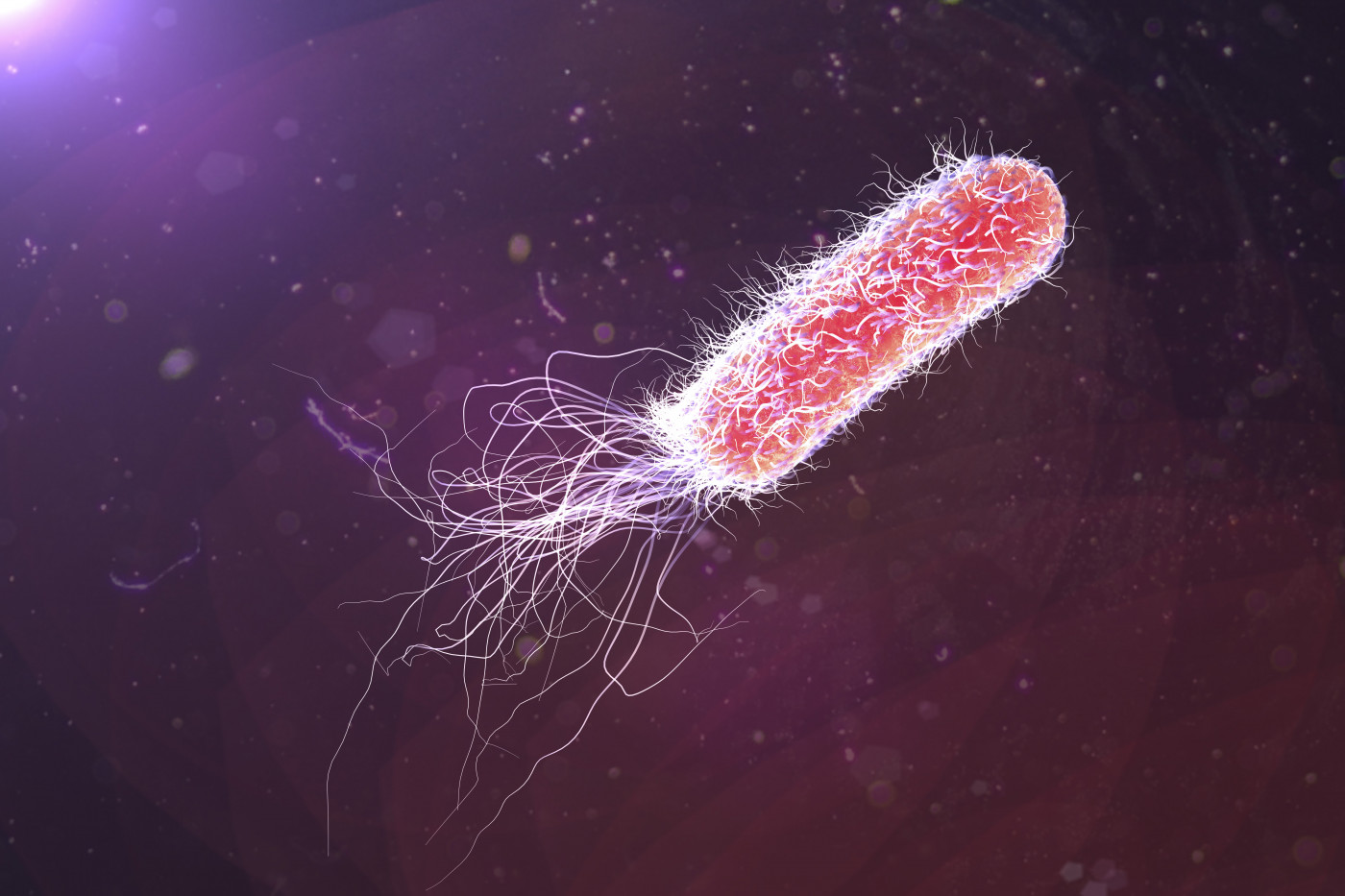
Combining the approved multiple sclerosis treatment glatiramer acetate with the antibiotic tobramycin improved its ability to kill antibiotic-resistant strains of Pseudomonas aeruginosa isolated from cystic fibrosis (CF) patients, new data show.
These results were shared in the presentation “The repurposed multiple sclerosis drug, glatiramer acetate, is an antibiotic resistance breaker in Pseudomonas aeruginosa strains from cystic fibrosis patients,” given by Ronan A. Murphy with Imperial College London at the recent 41st European Cystic Fibrosis Society (ECFS) Conference held in Belgrade, Serbia. The study was funded by the U.K.’s Cystic Fibrosis Trust.
Glatiramer acetate, manufactured and marketed under the brand name Copaxone by Teva Pharmaceuticals, was approved by the U.S. Food and Drug Administration (FDA) in 1996 to treat multiple sclerosis (MS). Since then, Copaxone has been approved for marketing in more than 50 countries worldwide.
An immunomodulatory injectable therapy, glatiramer acetate works to reduce the frequency of relapses in MS patients. The treatment consists of four basic amino acids (L-glutamic acid, L-alanine, L-tyrosine, and L-lysine), having a similar chemical identity to that of antimicrobial peptides.
In a previous study, researchers showed that glatiramer acetate has antimicrobial activity against P. aeruginosa, the most common pathogen found in CF patients and one marked as a critical priority for new antimicrobials by the World Health Organization.
In this study, the research team tested its potential in helping to overcome various P. aeruginosa strains that are resistant to antibiotics.
The team tested antibiotic sensitive and resistant strains of P. aeruginosa isolated from airway secretions of CF patients at the Royal Brompton Hospital, London.
The different strains were incubated with varying concentrations of tobramycin, a standard-of-care antibiotic used for P. aeruginosa infections, both in the presence or absence of glatiramer acetate (at a concentration of 50 µg/L).
Researchers incubated the cultures overnight and assessed the bacterial growth every hour.
Adding glatiramer acetate to tobramycin increased the killing of sensitive P. aeruginosa strains by 56.6%, results showed.
The tobramycin-resistant strains were also more effectively killed in the presence of glatiramer acetate, especially with higher doses of the antibiotic – the killing efficiency increased by 24.2% with 4 mg/L of tobramycin in one case, and by 71.2% in the presence of 8 mg/L of tobramycin in another cases.
“Glatiramer acetate is an antibiotic-resistance breaker of tobramycin for P. aeruginosa,” Murphy said in his presentation. “Co-administration of GA [glatiramer acetate]-tobramycin could allow dose reduction of antibiotic by up to 50% for the same effect,” he added.
This would result in a “reduction on antibiotic burden and potential side-effects,” Murphy concluded.
The researchers are also testing glatiramer acetate’s ability to work with other antibiotics, namely ceftazidime, ciprofloxacin, and colistin.