MRSA Difficult to Eradicate, Even With Multimodal Antibiotics, CF Study Finds
Up to one month of treatment with inhaled vancomycin, the antibiotic of choice for treating most methicillin-resistant Staphylococcus aureus (MRSA) infections, together with a combination of oral and topical antibiotics, failed to clear infection in cystic fibrosis (CF) patients at better rates than the antibiotic combination alone, results from a Phase 2 clinical trial show.
The study “Eradication of persistent methicillin-resistant Staphylococcus aureus infection in cystic fibrosis” was published in the Journal of Cystic Fibrosis.
The prevalence of MRSA in CF patients has increased in the past two decades, and it is estimated that currently 26 percent of CF patients in the U.S. are infected with MRSA.
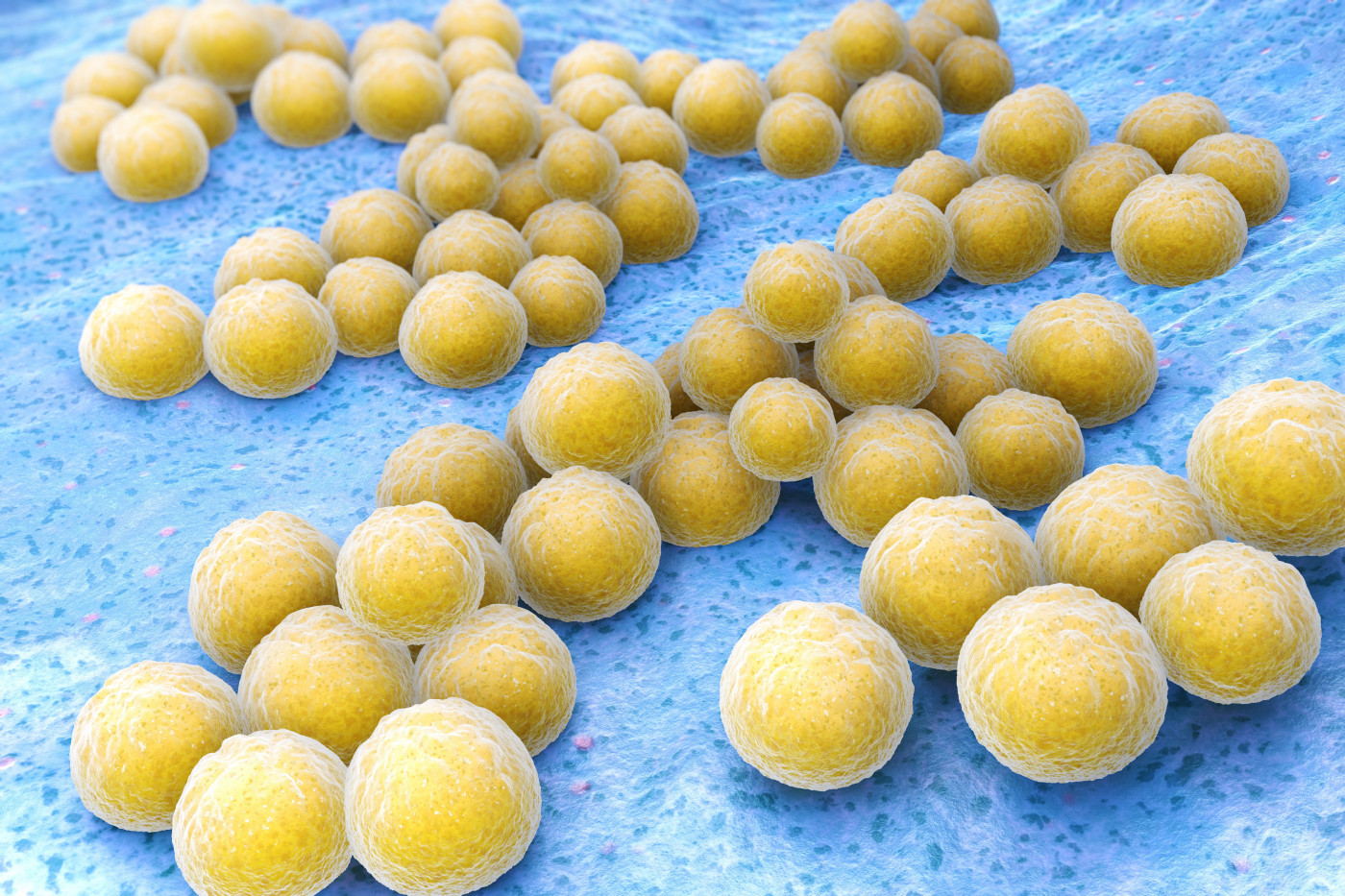
Staphylococcus aureus is the most prevalent bacteria in the airways of CF patients. MRSA is a particular challenge in CF due to its resistance to standard antibiotics used in the clinic.
Studies based on the U.S. Cystic Fibrosis Foundation Patient Registry (CFFPR) suggest that persistent MRSA infection is associated with worse outcomes in CF; 43 percent of the patients had a faster decline in lung function, which led to a lower survival, relative to CF patients without MRSA or to those in whom the infection was eradicated.
However, “while studies demonstrate that persistent MRSA infection in CF is associated with poor clinical outcomes, there are no randomized controlled studies informing management,” researchers wrote.
Previous studies suggested that aggressive antibiotic therapy is a potential approach to eradicate MRSA in CF patients, although these studies lacked appropriate controls.
So, researchers performed a randomized, double-blind, placebo-controlled Phase 2 trial (NCT01594827; the Persistent MRSA Eradication Protocol, or PMEP) to evaluate the safety and effectiveness of a 28-day eradication strategy — a combination of oral and topical antibiotics, with or without vancomycin — in CF patients with persistent MRSA infection.
Participants were randomized to treatment with a placebo or vancomycin, delivered via inhalation in doses of 250 milligrams (mg) twice a day, plus the combination of antibiotics. Patients were treated for 28 days and followed for three months.
The study’s primary objective (endpoint) was to assess the percentage of patients who became MRSA-free one month after completion of treatment, as shown by culture of sputum samples (material coughed-up from the airways).
Additional goals included changes in lung function (measured using the forced expiratory volume in one second, FEV1, referring to the volume of air that can be forced out in one second after taking a deep breath) from the beginning of the study up to the three months of follow-up, and changes on the Cystic Fibrosis Questionnaire-Revised (CFQR) focusing on the respiratory score, among other parameters.
The study recruited 29 CF patients — 14 were randomized to antibiotic therapy plus vancomycin and 15 to antibiotic therapy plus placebo. Four patients in the vancomycin group discontinued the study due to bronchospasm (restricted airflow due to abnormal contraction of the smooth muscle of the bronchi), so in the end a total of 25 patients were analyzed.
At the end of the 28-day treatment, 50% (five of 10) patients treated with inhaled vancomycin plus antibiotics were negative for MRSA, compared to 40% (six of 15) in the placebo-antibiotics group — a difference of only 10%.
One month after treatment completion (the study’s primary endpoint), there was no difference between the two groups; 20% of the patients in each group had a MRSA negative sputum culture test (two of 10 in the vancomycin group, and three of 15 in the placebo group).
Three months after completing treatment, there was still no statistically significant difference in MRSA eradication rate between the two groups – 20% in the vancomycin plus antibiotics group (two of 10), versus 13% in the control group (two out of 15).
Additionally, there was no difference in lung function and in the CFQ-R questionnaire between the groups at any time point analyzed.
Overall, the study supports how ”persistent MRSA infection is difficult to eradicate, even with multimodal antibiotics,” researchers wrote.
“The use of a single course of inhaled vancomycin may not lead to higher rates of MRSA eradication in individuals with CF and may be associated with bronchospasm,” the team concluded.
Of note, the Cystic Fibrosis Foundation funded this trial.







