Patient-derived Mini-organs Work as ‘Avatars’ to Test CF Treatments
Researchers in Australia are growing mini gut and lung “avatars” derived from cells of children with cystic fibrosis (CF) to predict their response to current and potential medications.
This platform may revolutionize the way clinicians treat CF patients, reducing the “trial-and-error” phase from the treatment process, and helping to develop personalized medicine.
CF can be caused by more than 1,700 mutations in the CF transmembrane conductance regulator (CFTR) gene. Most of these mutations result in little to no CFTR protein at the cell surface, where it controls salt and fluid secretion.
The development and approval of CFTR modulators to treat dysfunctional CFTR proteins have transformed CF patients’ lives by easing disease symptoms, improving quality of life, and increasing life expectancy.
Currently approved CFTR modulators — Symdeko (tezacaftor/ivacaftor), Orkambi (lumacaftor/ivacaftor), and Kalydeco (ivacaftor), all by Vertex Pharmaceuticals — target the more common CFTR mutations, covering 60% of CF patients. Yet, because everyone responds differently to medications, not all carriers of these mutations respond to treatment, adding to the other 40% of patients with rare mutations who still lack CF-specific therapies.
The high number of CF-causing mutations makes it impossible to develop a “one-size-fits-all” CFTR modulator. Also, the pricing of currently approved therapies (about $300,000 per patient per year) has been deemed excessive by the Institute for Clinical and Economic Review, a non-profit watchdog in the U.S.
Given the unmet need of a cost-effective method to identify who may respond to current and future treatments, researchers at the University of New South Wales (UNSW), in Sydney, Australia, developed the miCF AVATAR platform, which uses patient-derived mini-organs to assess the best medication for each patient.
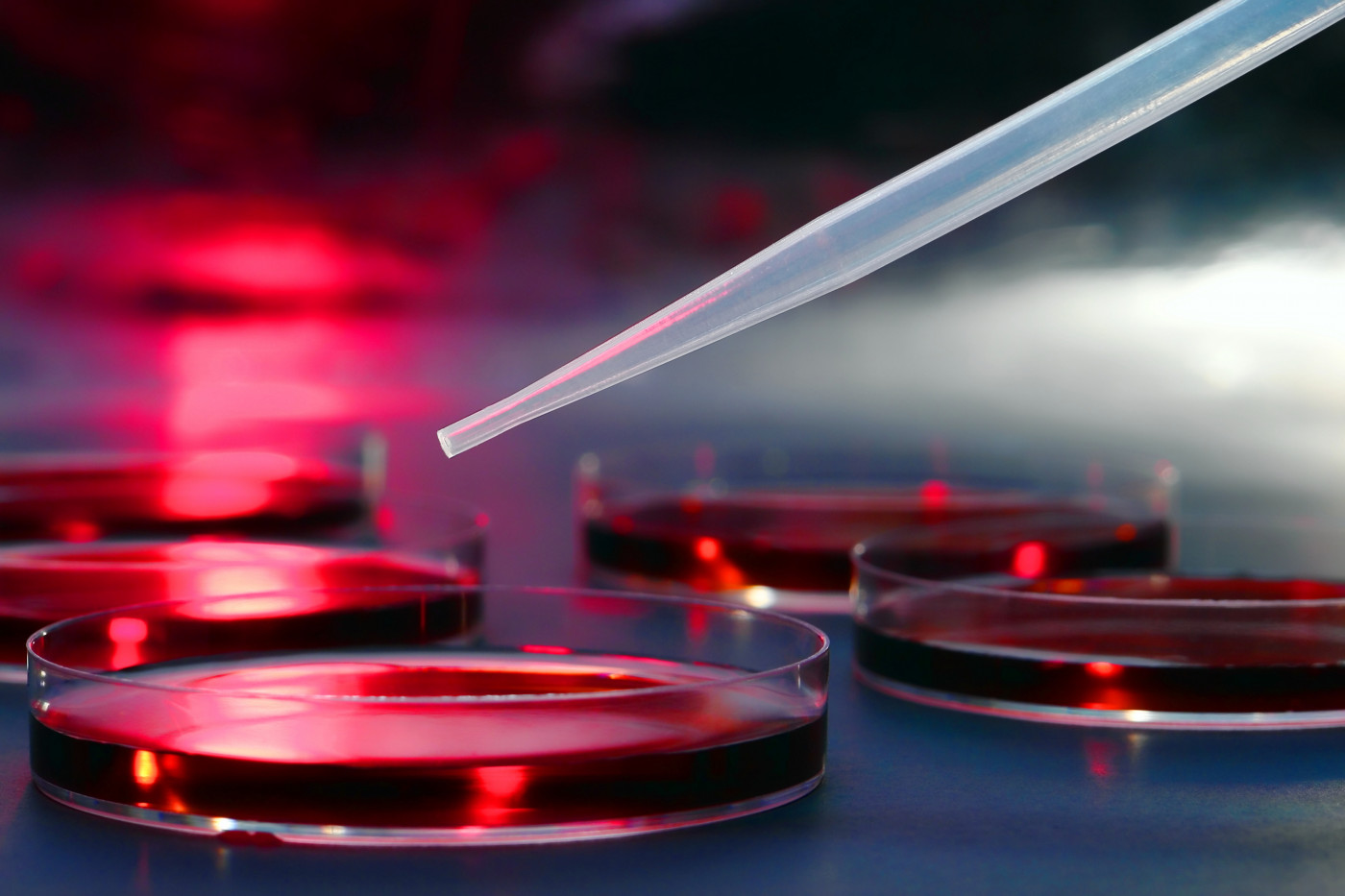
Patients’ stem cells are collected at 11 CF clinics across Australia, then sent to the Molecular and Integrative Cystic Fibrosis (miCF) Research Centre, where they are grown into miniature versions of the gut and lung — two organs highly affected by this disorder. These cells are grown in a gel-like substance, which allows the formation of 3D organ-like structures called organoids.
These mini-organs act as an “avatar” for each child, and since they can be expanded in the lab, millions of copies of the avatars can be used to test several medications.
Upon exposure to a treatment capable of restoring the function of the defective CTFR protein, the avatar swells up. The more it swells, the more likely the child will respond to that treatment.
Medications working in these avatars then could be recommended as target therapies for the patient.
These mini-organs are then frozen and preserved in the miCF biobank, so that they can be tested with new medications in the future.
The miCF biobank, launched in 2017, was established through collaboration between UNSW Sydney and the Sydney Children’s Hospital (SCH) Respiratory and Gastroenterology department. It relies on a national network of CF clinicians, scientists, and their institutions working together with the miCF Research Centre.
So far, three of the avatars identified as responsive to current CFTR modulators were from children with ultra-rare CFTR mutations, according to a UNSW press release.
Adam Jaffe, miCF Research Centre’s co-director and head of the School of Women’s and Children’s Health at UNSW Medicine, previously commented that this platform will help clinicians develop personalized treatment, ensuring children receive the best value healthcare with the right therapy.
“Similar personalised medicine platforms have shown remarkable success in other areas of healthcare, such as cancer, with CF platforms in use overseas. Moving away from a one size fits all model of care is vital if we are to improve the health and life expectancy of individuals with CF,” Jaffe said in a previous SCH press release.
“Our hope is that children with CF live to old age, and are only inconvenienced by taking a couple of pills a day,” Jaffe said.
The team also is working on potential ways to correct the defective CFTR protein by adding a correct copy of the CFTR gene to the cells.