AIT’s Inhaled Nitric Oxide Shows Potential in Fighting Bacterial Infection Prevalent in CF Patients
Inhaled nitric oxide (NO) was shown to be an effective antibacterial agent against Mycobacterium abscessus infection in preclinical studies, as well as in a pilot clinical trial, according to AIT Therapeutics.
The company discussed the latest data on its NO product in two poster presentations during the 3rd Annual World Bronchiectasis Conference held recently at Georgetown University in Washington, D.C.
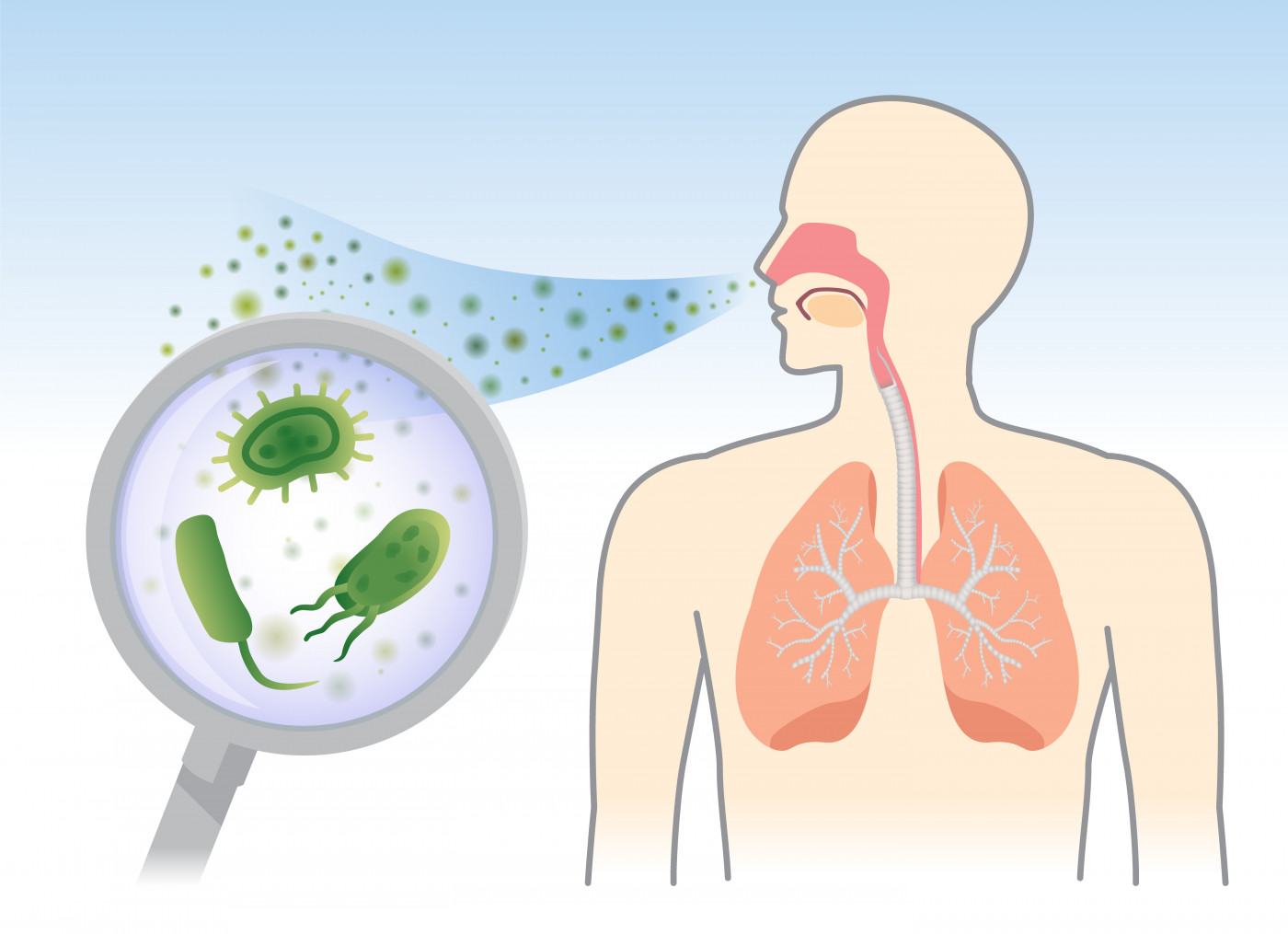
NO is a small molecule that is an important mediator of immune defense mechanisms against infections. The compound has been shown to have broad-spectrum antibacterial activity against several strains of bacteria that often infect patients with underlying lung diseases, including cystic fibrosis (CF).
In the first poster, “Anti-mycobacterial Activity of High-dose Nitric Oxide against Mycobacterium abscessus In Vitro,” researchers described the activity of NO against M. abscessus, an emerging multidrug-resistant nontuberculous mycobacteria (NTM) that has a high prevalence among CF patients.
The team cultured M. abscessus bacteria collected from a CF patient in artificial sputum, and exposed them to high doses of NO.
Results showed that the treatment could effectively prevent the growth of the bacteria and even promote their death, significantly reducing bacteria burden, an effect that was dependent on the level of NO concentration used. In addition, different multidrug-resistant clinical isolates of M. abscessus showed susceptibility to the lower of the tested NO doses.
Researchers also evaluated NO’s potential against Pseudomonas aeruginosa, another bacteria strain that often infects CF patients. The treatment not only showed it could significantly reduce P. aeruginosa burden, but it could do it faster and at a lower concentration than that reported for M. abscessus.
They are now planning to further evaluate NO’s effects on M. abscessus, when administered alone or in combination with other available therapies.
“Confirmation of the killing effect of nitric oxide in vitro on M. abscessus is uplifting. Add in the killing of Pseudomonas aeruginosa, a notoriously harmful pathogen in our CF population, and one can begin to have hope that NO may be the non-antibiotic anti-microbial we have been waiting for,” Andrew Colin, MD, director of the division of pediatric pulmonology at the University of Miami, said in a press release.
Results from a pilot clinical study were presented in a second poster, titled “Treatment of Refractory Mycobacterium abscessus Lung Infection with Inhaled Intermittent Nitric Oxide.”
In this study, researchers evaluated the therapeutic potential of inhaled NO against drug-resistant M. abscessus infection in a CF patient.
The patient, a 25-year-old woman, had an eight-year history of chronic drug-resistant M. abscessus infections with progressively deteriorating lung function. She received NO treatment under a compassionate use experimental treatment protocol approved by the U.S. Food and Drug Administration.
She received inhaled NO for a total of 21 days, delivered via a novel portable generator with a face mask developed by the company. For the first 14 days, she underwent five 30-minute treatments every 3.5 hours per day (during the day). The treatment frequency was reduced to three 30-minute sessions every 3.5 hours per day for the remainder of the 21-day treatment period.
Intermittent administration of highly concentrated NO was well-tolerated by the patient, with no significant treatment-related adverse effects reported.
Evaluation of her health status before and after the therapy showed she experienced significant improvements in several domains, particularly in physical, vitality, health perceptions, and respiratory domains, as determined by Cystic Fibrosis Questionnaire – Revised (CFQ-R) scores.
Inhaled NO also improved her lung function, shown by better results in forced vital capacity (FVC) and the six-minute walk test distance by the end of the treatment compared with the start of the study. Additionally, analysis of C-reactive protein levels and erythrocyte sedimentation rate showed that treatment with inhaled NO reduced inflammation.
“Following therapy, she was able to complete her degree and obtain a job,” the researchers reported.
Despite these positive health-related improvements, the researchers failed to detect any effects on M. abscessus, with no significant changes in bacteria load.
“Inhaled NO is a novel approach to severe NTM [nontuberculous mycobacterial] infection that may offer improvement in various parameters to patients with severe chronic infections,” they said. Still, “further investigation is required to determine the most effective concentration and treatment schedule to reduce mycobacterial burden and potentially achieve eradication.”
“Results from the treatment with our NO generator and delivery system were consistent with the results shown from our recently completed nine patient NTM study [NCT03208764] using cylinder gas,” said Steven Lisi, chairman and CEO of AIT Therapeutics.
AIT is planning to launch a pivotal study by the end of 2019 to evaluate the effectiveness of inhaled NO to clear NTM infections. This study is pending appropriate funding, and is expected to be conducted mainly in the home setting, Lisi said.







