S. aureus Bacteria Seen to Lose Resistance to Antibiotics When Combined with Rhamnolipids
Molecules used by a bacterial species against other microbes, called rhamnolipids, can bolster the ability of a standard antibiotic to penetrate treatment-resistant strains of Staphylococcus aureus by essentially making holes in the membrane of its cells, a new study confirms.
The study, “Chemical Induction of Aminoglycoside Uptake Overcomes Antibiotic Tolerance and Resistance in Staphylococcus aureus,” was published in the journal Cell Chemical Biology.
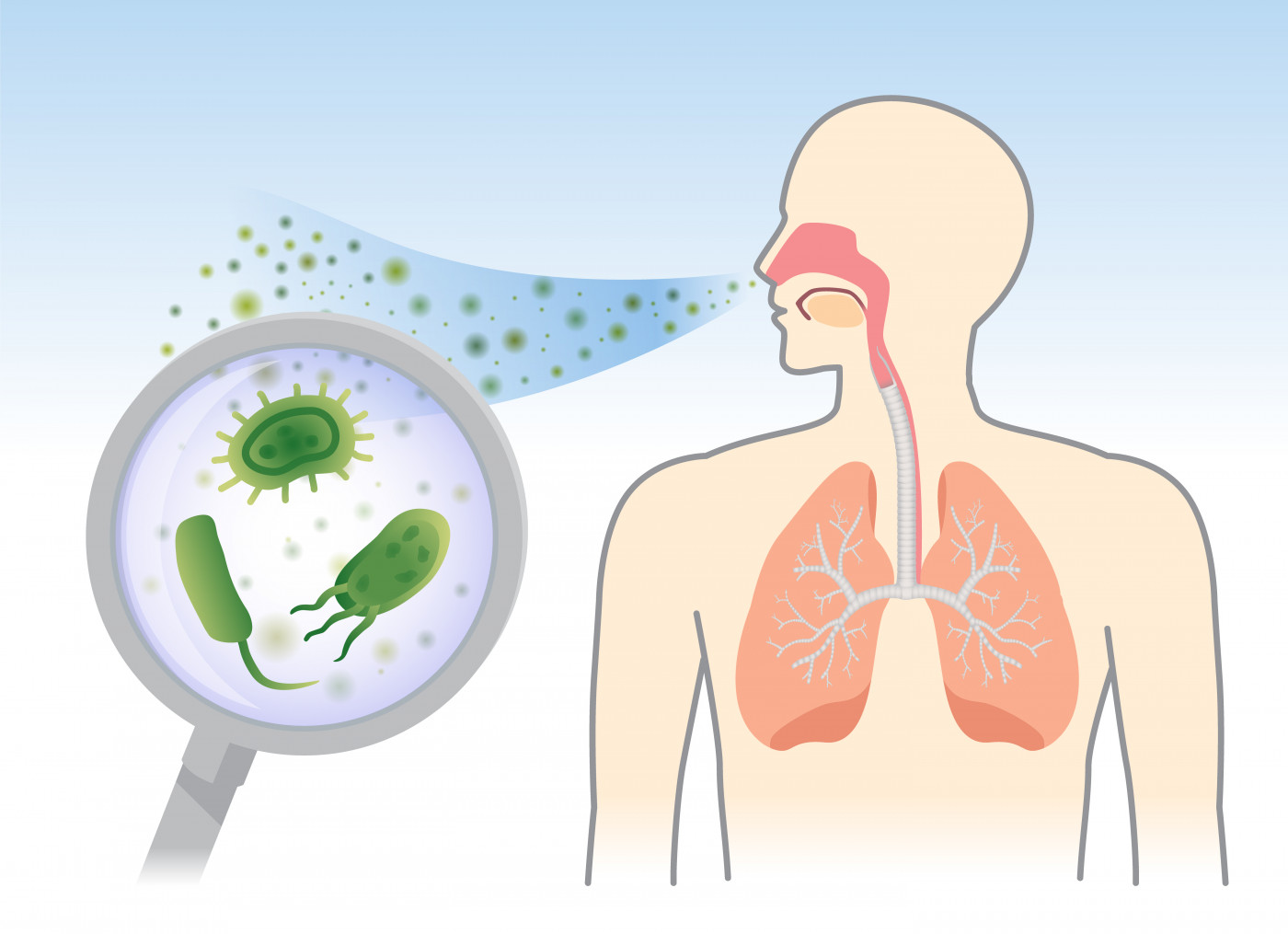
Staphylococcus aureus (S. aureus) bacteria can cause serious infections that are often resistant to antibiotic treatment. Bacteria can acquire resistance by genetic mutation, but also by living in environments that make them less vulnerable to antibiotics, such as the low-oxygen zones in the mucus-filled lungs of people with cystic fibrosis (CF).
In these environments, broad-spectrum aminoglycoside antibiotics, like tobramycin, are not effective because they cannot penetrate the bacterial membrane.
A research team at the University of North Carolina on 2017 identified a class of biochemicals called rhamnolipids (RLs) that were produced by another bacterial species, Pseudomonas aeruginosa. These RLs were seen to enhance tobramycin’s potency against standard test strains of S. aureus. Rhamnolipids are thought to act as natural weapons against other wild bacteria by making holes in cell membranes.
To investigate further, the team tested RLs together with tobramycin treatment in several S. aureus strains that are antibiotic-resistant. These included: 1) a strain that grows in low-oxygen environments; 2) persistent strains that grow slowly, making them more tolerant of antibiotic treatment; 3) strains that have genetically acquired resistance to another aminoglycoside antibiotic, methicillin; and 4) strains isolated from CF patients that are tobramycin-resistant.
Interested in Cystic Fibrosis research? Sign up for our forums and join the conversation!
Researchers grew these strains in the presence of tobramycin with and without RLs, and measured S. aureus growth.
Results showed that strains normally resistant to tobramycin treatment were rapidly killed in the presence of rhamnolipids in a dose-dependent manner. This enhanced antibacterial effect was observed even at low RL doses. This extended to other aminoglycoside antibiotics such as gentamicin, amikacin, neomycin, and kanamycin.
However, these effects were specific to aminoglycosides. RLs did not enhance the potency of other types of antibiotics, such as ciprofloxacin, rifampicin, oxacillin, and tetracycline.
Researchers also tested the tobramycin-RL combination in other types of bacteria, and found similarly enhanced activity against Enterococcus faecalis, Bacillus subtilis, Listeria monocytogenes, and Clostridioides difficile (C. difficile). The authors noted a dramatic effect of tobramycin-RL treatment against C. difficile, a major cause of serious diarrheal illness.
Finally, the team confirmed that RLs worked by making holes in the bacterial cell membrane, making the membrane more permeable and allowing the antibiotics to penetrate the cell.
Based on these results, the researchers suggested that the tobramycin-RL combination represents a “promising new approach for resolving chronic or relapsing infection, improving patient health, and slowing the spread of resistance,” they wrote.
The team also emphasized that “this combinational therapy demonstrates remarkably potent bactericidal activity against persisters, a bacterial population that is notoriously tolerant to killing, regardless of antibiotic class.”
“Tobramycin doses that normally would have little or no effect on these S. aureus populations quickly killed them when combined with rhamnolipids,” Lauren Radlinski, the study’s first author, said in a university news article written by Mark Derewicz.
The next step will be to evaluate other rhamnolipid variants to find the combination that is most effective at killing bacteria, while minimizing the side effects on human cells.
“There’s a great need for new ways to kill bacteria that tolerate or resist standard antibiotics, and to that end we found that altering membrane permeability to induce aminoglycoside uptake is an extremely effective strategy against S. aureus,” Brian Conlon, PhD, an assistant professor at the UNC School of Medicine and the study’s senior author, concluded.







