Long-term effects of Trikafta on lungs’ microbial dynamics explored
Microbe diversity, lung function improves, but bacterial burden persists
Written by |
A high burden of infection-causing bacteria persisted in the lungs of people with cystic fibrosis (CF) who were treated with Trikafta (elexacaftor/tezacaftor/ivacaftor) in a recent study, despite an increase in the overall diversity of microbes and improvements in lung function being seen.
The changing dynamics of this microbial environment and their effects on lung function with long-term treatment remain to be explored, the study’s researchers said in “Longitudinal microbial and molecular dynamics in the cystic fibrosis lung after Elexacaftor–Tezacaftor–Ivacaftor therapy,” which was published in Respiratory Research.
“Further study of changes in the airway microbiology and biochemistry of [people with CF] taking highly effective modulators will reveal the future infection landscape of this rapidly improving chronic lung disease,” they wrote.
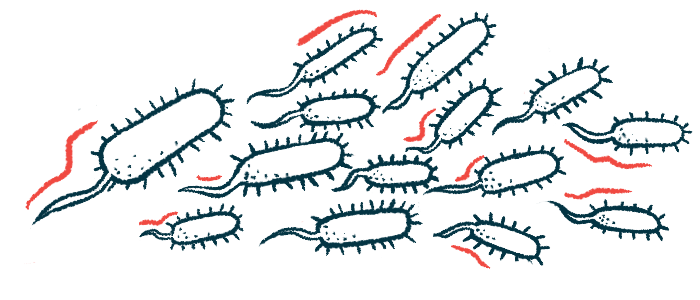
In the lungs of people with CF, the microbiome — the collection of bacteria, fungi, and viruses living in the respiratory tract — is dysregulated. The thick and sticky mucus that builds up there promotes an environment where opportunistic pathogens, such as Pseudomonas aeruginosa, grow and cause infections that drive declines in lung function. Over time, these harmful microbes become dominant and the overall diversity of the lung microbiome is diminished.
Trikafta, an approved triple-combination CFTR modulator therapy from Vertex Pharmaceuticals, was found in a recent study to quickly reduce the density of these harmful microbes in the airways within the first month, which remained stable for up to six months in some patients. It’s also been shown to increase overall microbial diversity.
Effects of Trikafta on microbiome
Research on other CFTR modulator therapies has found that after an early reduction in lung infections, microbial growth had a resurgence later on, leading researchers here to examine long-term changes in the microbial makeup of the respiratory tract among seven CF patients using Trikafta compared to nine who didn’t. They also examined the profile of metabolites, the byproducts of chemical reactions, which are also altered in the CF lungs and can contribute to microbial growth.
Patients collected samples of sputum, or phlegm, at home. Trikafta-treated patients collected samples over an average of 267 days, or nearly nine months. They started collecting samples an average of 236 days (almost eight months) after starting Trikafta.
A total of 162 samples were collected from those patients, whereas 630 samples were collected from those not on Trikafta. That difference can be attributed to the fact that Trikafta therapy reduces sputum production, the scientists said.
Patients treated with Trikafta saw improvements in lung function that weren’t significantly different than those seen in previous groups of patients treated at the researchers’ clinic. The daily increase in microbial diversity was higher in Trikafta-treated patients than untreated patients. The diversity of metabolites more rapidly increased on Trikafta also.
Still, these dynamics varied. Microbial and metabolic diversity in the sputum increased linearly over time since starting treatment for five of the seven patients, but were more stable in the other two.
“A progressively changing microbiome and metabolome is occurring in those on CF within the first year of therapy, though not in all subjects,” the researchers wrote. “This may indicate personalization and variation in the longer-term response to [Trikafta], with some subjects’ infections becoming relatively static, while others continue to change with time.”
Little change in bacterial load
Despite improvements in lung function, infections with disease-causing, or pathogenic, bacteria persisted, including Pseudomonas, Burkholderia, and Staphylococcus. There was little change in the abundance of these bacteria or total bacterial load over time.
Using antibiotics during the study may have influenced the findings. Analyses indicated that while the antibiotic azithromycin may have impacted microbial profiles, no others did, “so this impact is likely minimal overall,” the scientists wrote.
Analyses also showed the microbiome took on more neutral dynamics with Trikafta, a profile more consistent with a healthy microbiome. Those dynamics imply the original increase in microbial diversity after Trikafta could begin to stabilize over time, however.
It remains to be seen if the Trikafta-exposed lung microbiome will achieve a “new-steady state” or if it will “constantly improve, with pathogens progressively eliminated with time,” the researchers said.