Blood Levels of Fibrocytes Unusually High in Children With CF: Study
Written by |
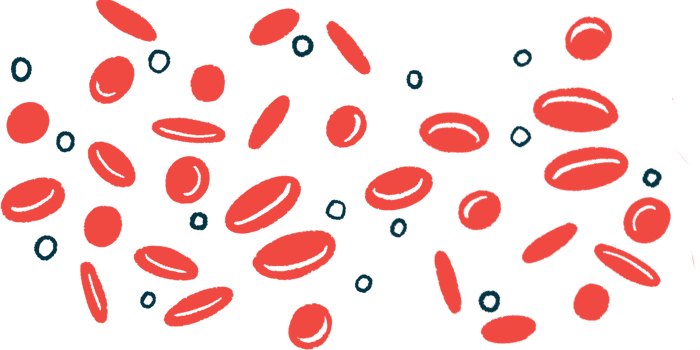
Children with cystic fibrosis (CF) have significantly higher level of fibrocytes — cells associated with diseases marked by fibrosis or scarring — in their bloodstream relative to healthy children, a study reported.
Findings further revealed that these fibrocyte levels were lower during CF exacerbations than stable disease, and lower in children with poorer lung function, possibly indicating these cells had migrated from the blood to lung tissue.
The study, “Circulating Fibrocyte Level in Children with Cystic Fibrosis,” was published in the journal Pediatrics International.
CF occurs as a result of defects in the CFTR gene that codes for a chloride ion channel, disrupting the movement of water and salts in and out of cells.
Structural lung damage in CF patients begins to develop around age 5 due to chronic infections and inflammation, although lung damage without structural changes begins earlier.
Fibrocytes circulating in the bloodstream can migrate to injured or inflamed tissues and transform into mature fibrocytes that are similar to fibroblasts, cells that secrete collagen proteins that maintain the structure of many tissues and are involved in wound healing.
Studies have found high levels of fibrocytes in the blood and lung tissue of patients with diseases such as idiopathic pulmonary fibrosis and chronic obstructive pulmonary disease, the study noted, and recent evidence has shown fibrocyte accumulation in CF patients with end-stage lung disease.
“These data suggested … [that] circulating fibrocytes might have [a] potential role in CF lung disease,” its scientists wrote.
Researchers in Turkey looked at fibrocyte levels in 39 children with CF (median age, 9), analyzing the link between such levels and imaging findings, pulmonary function tests and pulmonary exacerbations. They also assessed differences among the 31 children with stable disease and the eight with a CF exacerbation during the study’s year (May 2018–June 2019).
Exacerbation was defined as having new crackles, increased cough and sputum, a relative decline of more than 45% in their weight-for-age percentile, increased hemoptysis (spitting of blood coming from the airways), high fever, at least 10% reduction in lung function, and new radiological findings suggesting lung infection.
CF patients were compared with 20 healthy children of similar age (median age, 10) and sex serving as a control group.
Children with stable disease had significantly higher numbers and percentages (among cells with the CD45 surface marker) of circulating fibrocytes compared with patients with exacerbations.
Overall, CF patients showed significantly higher fibrocyte numbers and percentages than did the control group.
Levels of fibrocytes in children with exacerbations were also higher when their disease was stable (a median absolute number of 106605/ml) than during a flare (median of 4783/ml), a point the researchers found “interesting.”
This decrease in circulating fibrocytes during exacerbations suggests that fibrocytes had migrated to tissue rather than remaining in the bloodstream, they noted, recommending further investigation.
“Circulating fibrocytes which migrate to the lung tissue due to the prolonged damage and inflammation might have [a] potential role in the tissue repair and/or tissue damage of CF patients,” the researchers wrote.
Pulmonary function tests performed on 25 patients found a forced expiratory volume in one second (FEV1; how much air a person can forcibly exhale) of less than 80% in eight children. Notably, the 17 patients with FEV1 values greater than 80% had higher median circulating fibrocyte numbers than did those with a lower FEV1.
The scientists also looked at forced vital capacity (FVC), the total amount of air exhaled during the FEV test. They found that six patients had an FVC of less than 80%, while 19 others had a higher FVC. Fibrocyte numbers were again lower in the patients with a poorer FVC, but this difference was not statistically significant.
Using both FEV1 and FVC values, data showed a significant decrease in circulating fibrocytes in patients who had both low FEV1 and FVC as compared with those with normal values on lung function tests.
Researchers then grouped the children based on high-resolution computed tomography imaging findings, as assessed using the Shwachman-Kulczycki scoring system of disease severity in CF (higher scores indicate better clinical status).
Nineteen patients had scores in the 0–15 range indicating severe to mildly affected (group 1) and 20 had scores of 16–25 considered good to excellent (group 2). Fibrocyte counts for patients in group 1 were significantly lower than those in group 2.
“To the best of our knowledge, there is only a single recent study analyzing circulating fibrocyte count in patients with CF, therefore, these findings are expected to shed light on future studies,” the investigators wrote. “Further studies are also needed to determine the role of circulating fibrocytes in the [development] of CF.”