Lung Airway Chip Accurately Models Cystic Fibrosis
Written by |

For the first time, many features of cystic fibrosis (CF) were modeled accurately in a human Lung Airway Chip lined with cells from CF patients, which included enhanced mucus secretion, inflammation, and microbial infections, a study has shown.
This “organ-on-a-chip model” of the disease may support the rapid development of much-needed therapies, with the potential of personalized medications for CF patients.
“Now that we are able to accurately model CF [disease], including microbiome and inflammatory responses, in human Airway Chips, we have a way to attack challenges that are important to CF patients,” Donald Ingber, MD, PhD, said in a press release. Ingber is study lead and founding director of the Wyss Institute for Biologically Inspired Engineering at Harvard University in Massachusetts.
The study, “Modeling pulmonary cystic fibrosis in a human lung airway-on-a-chip,” was published in the Journal of Cystic Fibrosis.
In CF, a faulty cystic fibrosis transmembrane conductance regulator (CFTR) protein impairs the function of cells that line the airways and digestive tract. As a result, these cells become surrounded by abnormally thick mucus, increasing susceptibility to infections and inflammation.
About 90% of CF patients carry the CFTR mutation called F508del, which can be treated with certain medications. Despite these advances, the long-term impact on lung inflammation remains unclear. Furthermore, in about 10% of cases, the disease is caused by other CFTR mutations for which there are no targeted treatments.
There is a lack of patient-derived, cell-based (in vitro) models that mimic underlying CF biology and can be used to screen potential medicines rapidly. That is a barrier to developing much-needed therapies.
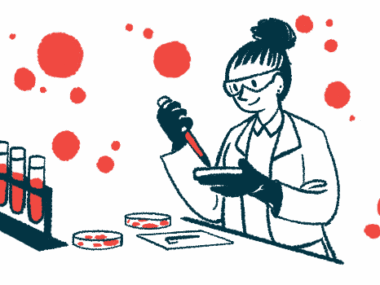
Now, a research team led by Ingber has developed a Lung Airway Chip device — the size of a USB memory stick — that resembles key hallmarks from CF patients more accurately compared with other in vitro systems used so far. The work was supported by a grant from the Cystic Fibrosis Foundation.
“The bundled capabilities of this advanced in vitro model can help accelerate the search for drugs that may dampen the exaggerated immune response in patients, treat them with more personalized therapies and, help solve problems that CF patients face every day which cannot be addressed by existing treatments,” Ingber said.
The team created Airway Chips by growing cells that line the airways — bronchial epithelial cells — isolated from CF patients or healthy individuals in one of two parallel-running hollow channels under air to mimic the lung’s air-transporting environment.
In a second channel, separated from the first channel by a porous membrane, a human blood vessel was recreated using cells from the lung environment, which were supplied with a blood substitute.
Both the healthy and CF cells formed tight single layers covering the entire length of the airway channels and had cilia — hairlike structures that extend from the cell surface that move debris and microbes out of the airways.
Experiments showed that, compared with chips lined with healthy cells, CF Airway Chips had a higher number of ciliated cells and a faster ciliary beat frequency (speed of cilia movement).
Microscopic analysis showed that mucus accumulated above the cell layer and staining experiments confirmed the CF Airway Chips generated more abundant mucin accumulation than healthy chips. In addition, the CF chips also exhibited a greater percentage of area covered by MUC5AC, a major protein component of mucus.
“This first microphysiological model of a CF airway closely mimics what we know from airways in CF patients,” co-first author Ratnakar Potla, PhD, said. “Maintaining the typical composition of all relevant cell types, it developed a thicker mucus layer, and its ciliated cells exhibit higher densities of cilia that beat at a higher frequency compared to Airway Chips created with airway cells from healthy individuals.”
CF lungs are characterized by enhanced inflammation. Consistently, compared with healthy chips, the CF Airway Chips showed a significant increase in the pro-inflammatory signaling protein interleukin-8 (IL-8).
To explore the inflammatory response of the chips, the team flowed immune cells through the recreated blood vessel channel. The immune cells adhered to the cells that lined the blood vessels and migrated through the porous membrane to the lung cell surface in both healthy and CF chips. Consistent with increased IL-8 levels, the number of immune cells that adhered to cells and migrated through the membrane was significantly higher in CF chips.
“Importantly, these pathological [disease-related] changes were accompanied by an enhanced inflammatory response in the modeled CF bronchial epithelium that is much like the one observed in CF patients,” Polta added.
Finally, to mimic infection by Pseudomonas aeruginosa — bacteria that frequently colonize CF airways — fluorescently labeled bacteria were introduced to the chips.
Twenty-four hours later, P. aeruginosa was detected in higher numbers in the CF-specific mucus than in mucus in healthy Airway Chips. As a result, the levels of pro-inflammatory signaling proteins were increased further, with more pronounced adhesion of immune cells to blood vessel walls in CF Airway Chips.
“In conclusion, the human CF Airway Chip reproduced for the first time, and with high fidelity, many of the structural, biochemical, and [disease-related] features of the human CF lung airway and its response to pathogens and circulating immune cells in vitro,” the scientists wrote. “Although the results shown here that were obtained with the CF Airway Chip reproduce many features of the diseased lung airway of CF patients, this model has room to be improved.”
The team noted that CF Lung Airway Chips could be created using airway cells, blood vessel cells, and immune cells isolated from the same patient.
“For this proof-of-concept study, we have only used CF-specific bronchial airway cells from patients carrying the frequent [F508del] CFTR mutation. But different CFTR mutations may also affect the function of endothelial and immune cells and differ in their effects,” said co-first author Roberto Plebani, PhD.
“By developing a panel of patient-specific Airway Chips using cells from patients with different mutations, and also by directly measuring the activity of differently compromised CFTR ion channels on-chip, drug responses and efficacies could be investigated in a highly personalized manner,” he added.