Vitamin D, calcium, and phosphate levels need yearly check: Study
Deficiencies seen in 'essential nutrients' in small patient group of various ages
People with cystic fibrosis (CF) can have abnormal levels or metabolism of three “essential nutrients” — vitamin D, calcium, and phosphate — even when using pancreatic enzyme replacement therapy (PERT) and taking dietary supplements, a small study suggests.
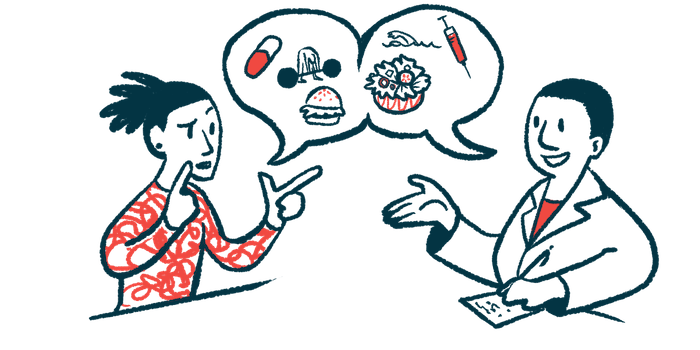
“The findings of this study have many practical implications in clinical practice and support the need to evaluate dietary, serum [blood], and urinary [calcium, phosphorus, and vitamin D] levels at least annually,” its researchers wrote.
The study, “Calcium, Phosphorus, and Vitamin D Levels in a Series of Cystic Fibrosis Patients: A Cross-Sectional Study,” was published in the International Journal of Molecular Sciences.
Calcium, phosphorus and vitamin D insufficiency can affect growth
Besides impaired lung function, mutations in the CFTR gene — the cause of CF — often result in exocrine pancreatic insufficiency (EPI). EPI refers to the pancreas’ inability to release sufficient digestive enzymes to break down food in the intestines, leading to poor nutrient absorption.
Proper absorption of calcium and phosphorus, together with vitamin D, are key for normal development and growth. These nutrients also play important roles in processes that include nerve cell activity, cell repair, and inflammation.
To better understand how the body may be affected by a lack of these three nutrients, researchers in Spain conducted a cross-sectional analysis, which looks at data at a single point in time, of CF patients followed at University Clinical Hospital of Valladolid.
In total, 17 children, adolescents, and adults (mean age of 14.8, 59% female) were included, all carrying F508del, the most common CF-causing mutation. Most participants were compound heterozygous, meaning they had this mutation in one gene copy and a different mutation in the other copy. The others were homozygous, as both CFTR gene copies had F508del.
Two patients were obese, as assessed by waist-for-height index, and two others were overweight. Undernutrition was detected in 12% of patients, but none had impaired growth.
Homozygous patients had significantly better tricep skinfold measures — a measure of fat reserves based on upper arm muscle circumference — and polyunsaturated fats consumption (20.4% vs. 15.1% of dietary reference intake or DRI). There fats are commonly present in nuts, seeds and fish.
Likewise, these patients showed a markedly higher intake of vitamin C (270% vs. 110% of DRI), vitamin D (1,259% vs. 243% of DRI), and iodine (67% vs. 45% DRI) than did heterozygous patients. Their blood urea nitrogen levels, a measure of kidney health, also were higher, 41.5 vs. 28 mg/dL.
In contrast, heterozygous patients had significantly higher mean levels of transferrin (274 vs. 231 mg/dL), a protein involved in iron metabolism, and of hemoglobin, 14.9 vs 13.5 mg/dL, which is responsible for delivering oxygen to tissues. White blood cells, platelets (tiny blood cells involved in blood clotting), and the immunoglobulin, or antibody, IgG3 also were elevated.
Respiratory insufficiency was found in 59% of the patients, as assessed by forced vital capacity and forced expired volume in one second. A majority, 76%, also had EPI, as assessed by a fat-absorption coefficient that reflects how well the body is absorbing fats from food. Patients with EPI had a significantly higher body mass index (BMI), a measure of body fat.
Those with lung infections positive for the fungus Candida spp., or the bacteria Pseudomonas aeruginosa or Staphylococcus aureus had a significantly lower intake of vitamin D than those without these infections. Most patients, 53%, played sports and 59% were active or very active.
Protein content was high in all the patients’ diets, and 47% had a diet high in calories. A high-fat diet was common, consumed by 82%, including 59% with a cholesterol-rich diet.
Protein metabolism, assessed by a measure called nitrogen balance that compares intake to excretion, was considered low.
Overall, 82% of the patients (15) had a low calcium/magnesium intake ratio. And, despite pancreatic enzyme replacement therapy and vitamin supplements, a deficiency was seen in vitamins A, E, and, especially troubling, vitamin D.
“Our patients were at increased risk of vitamin D deficiency (88%) despite high dietary vitamin D intake, supplementation, and PERT treatment,” the researchers wrote, adding that “[vitamin D] insufficiency is still a problem in CF patients.”
Vitamin C deficiency was found in seven patients and zinc deficiency in four. Three patients had high C-reactive protein, and two had a high erythrocyte sedimentation rate; both are markers of inflammation.
Levels of vitamins C, D, and E and of iron were not associated with their intake. Calcium levels were normal.
Three patients had low phosphate, a key electrolyte that constitutes about 1% of the total body weight and is a component of cell membranes, DNA, RNA, and proteins. High alkaline phosphatase, a sign of liver damage, was seen in 13 patients. Additionally, five participants (29%) had an excess of calcium and 11 of phosphate in their urine.
Statistical analysis showed that calcium, phosphate, and vitamin D levels significantly correlated with several parameters, such as BMI, diet, and physical activity, as well liver, kidney and immune functions.
Larger studies are needed to assess “the necessary and appropriate amount of supplementation for effective prevention with personalized nutritional recommendation,” the researchers concluded.