Gene Expression Patterns in Blood May Lead to Patient-tailored CF Treatment, Study Finds
Written by |
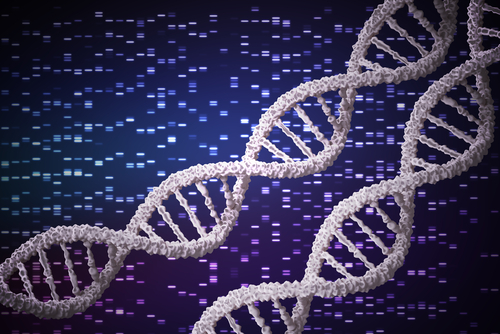
Researchers tested blood samples from cystic fibrosis (CF) patients and identified distinct gene expression patterns that could lead to patient-tailored treatments, a study reports.
The study, “Identification of molecular signatures of cystic fibrosis disease status using plasma-based functional genomics,” was published in Physiological Genomics.
To better understand CF disease progression and ultimately improve patient care, researchers at Stanley Manne Children’s Research Institute at Ann & Robert H. Lurie Children’s Hospital of Chicago gathered blood samples from CF patients and assessed the sequence and levels of a selected set of genes. The genetic data obtained was then associated with patient-specific clinical history based on medical records, and compared with gene expression patterns from healthy individuals.
The research revealed that CF-specific genetic patterns could be linked to clinical outcomes in patients.
“Our findings pave the way to precision medicine for cystic fibrosis patients, eventually helping us match treatment to each patient’s unique genomic pattern of disease,” Hara Levy, MD, lead author and associate professor of pediatrics at Northwestern University Feinberg School of Medicine, said in a press release.
Patient-tailored treatments would be important not only for the early management of CF, but also for the management of related complications, including inflammation of the airways due to infections, or issues related to the function of the pancreas.
“Our study was the first to identify molecular signatures of cystic fibrosis from a blood test taken during a routine clinic visit, giving us a baseline. Greater understanding of these molecular signatures may lead to unique molecular markers that could help us intervene earlier … allowing us to provide more focused treatment,” Levy said.
According to Levy, a patient-tailored therapeutic approach would represent a big “improvement over the one-size-fits-all treatment approach we currently have for patients with cystic fibrosis.”
Therapies directed against the defective CFTR gene, which is the primary cause of CF, are available. But the relationship among CFTR dysfunction, inflammation, and disease progression is unclear, which limits CF prognosis, treatment strategies, and assessments of patient response to treatment.
Consequently, the identification of molecular patterns in CF patients might clarify disease causes, symptoms, and progression. For example, it could help researchers to better understand the susceptibility of CF patients to chronic lung infections, despite their functional immune system.
“We are now trying to discover why patients with cystic fibrosis become infected so easily,” Levy said. “We are taking a closer look at the immune cells that make up many of the molecular signatures we found in cystic fibrosis.”
Nonetheless, more research is needed before precision medicine reaches the clinic.
“With more research, a blood test to gather genomic specifics of each patient’s disease might be available in the clinic within the next five years,” Levy said. “Precision medicine will revolutionize care for cystic fibrosis patients.”