MRSA infections linked to worse outcomes for children with CF
Infections associated with more antibiotic use, lung damage: Study
Written by |
In young children with cystic fibrosis (CF), infections with methicillin-resistant Staphylococcus aureus (MRSA) are linked to more antibiotic use, worse lung function, and more lung damage by early school age, according to a study led by researchers in Brazil.
Because infections with MRSA appear to indicate more severe disease and can be serious and difficult to treat, doctors should design a clear and standardized plan to eliminate these bacteria, researchers say, especially since treatment hasn’t been consistent everywhere.
“At a time of great optimism for individuals with CF fuelled by the discovery and increasing availability of CFTR modulators, maintaining the health of young people with CF to maximize their benefits from these new medications and reduce their daily treatment burden is crucial,” researchers wrote.
The study, “The bad bug: early MRSA infections in children with CF are associated with worse respiratory outcomes,” was published in Respiratory Medicine.
In CF, thick mucus builds up in the airways, leading to respiratory symptoms and making it more likely to develop infections such as those caused by MRSA. While these infections are a common problem for older patients with advanced disease, not much is known about MRSA in children.
Study included 81 children with CF
This study included 81 children diagnosed with CF, of whom 32 (39.5%) had MRSA detected in their airways before the age of 5 years. The first time they tested positive for MRSA varied widely, with some as young as 2 months, and others nearly 5 years old.
Nearly two-thirds (62.5%) received antibiotics against MRSA for a median of 14 days, and seven (21.9%) were admitted to the hospital. Before they tested positive for MRSA, children had already been hospitalized, and they had a median of two hospital stays and been on antibiotics for a median of 71 days (more than two months).
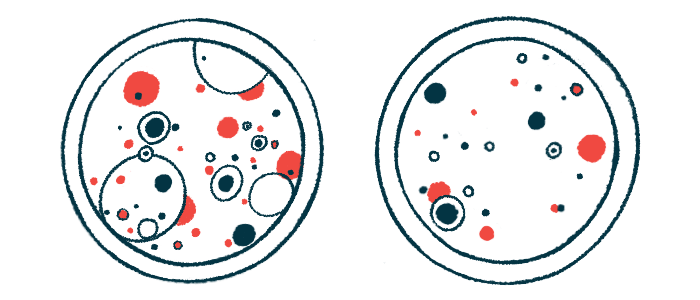
When comparing children with MRSA versus those without MRSA, both groups were similar in age at their first consultation, as well as in the type of CF-causing genetic mutations they had. However, children with MRSA had significantly higher levels of chloride in sweat. The sweat test is the gold standard for confirming a CF diagnosis and is also used to monitor the disease and response to treatment.
Children with MRSA had worse lung function by the time they were 6 or 7 years old. Their chest CT scans also had higher scores for bronchiectasis, meaning more lung damage was visible. Bronchiectasis occurs when the airways become irreversibly widened and damaged, often due to repeated infections.
Testing positive for MRSA before 5 years of age was linked to an average 10.1% decrease in forced expiratory volume in one second (FEV1), which measures the maximum amount of air that can be breathed out in one second. A lower FEV1 indicates worse lung function.
Lower FEV1 was linked to more infections with another type of bacteria called methicillin-sensitive Staphylococcus aureus — which differ from MRSA in their degree of antibiotic resistance — and more rounds of antibiotics.
While these findings “cannot define a relationship of causality between MRSA colonization and bronchiectasis or worse lung function results, [they] provide insight into the associations between early MRSA infection and CF lung disease outcomes,” the researchers wrote.
“Our study has limitations related to its sample size and retrospective nature, which may have restricted the detection of other clinical outcomes associated with early MRSA isolation,” they added.