Pulmonary Artery Measurements Used to Identify Pulmonary Hypertension in CF Patients
Pulmonary artery enlargement is linked to pulmonary hypertension (PH) and lower survival among patients with severe cystic fibrosis (CF), according to a recent review of patient records.
The study reporting the findings, titled “Pulmonary artery enlargement is associated with pulmonary hypertension and decreased survival in severe cystic fibrosis: A cohort study,” was published in the journal PLoS One.
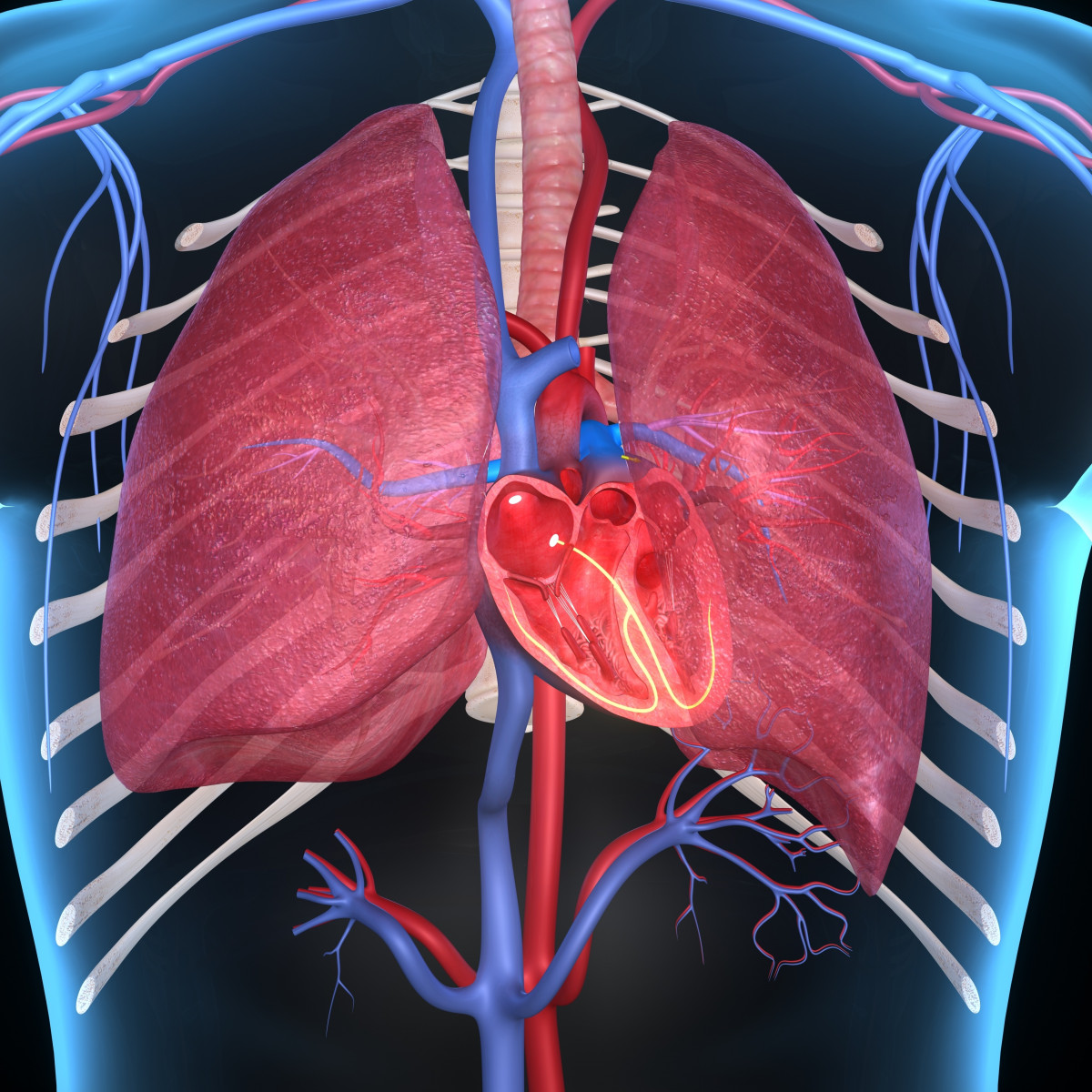
PH is known to limit survival in CF patients, but the gold standard method to confirm the disease, called right heart catheterization (RHC), is an invasive technique that cannot be used repeatedly in patients with chronic lung diseases such as CF.
PH can also be diagnosed by comparing the diameter of the pulmonary artery (PA) with that of the ascending aorta, a ratio known as PA:A. This measurement can be made via computed tomography (CT), a noninvasive imaging technique.
A group of researchers from the University of Alabama at Birmingham (UAB) reasoned that PA:A could therefore be useful in identifying PH in severe CF cases, and that pulmonary artery enlargement (meaning a PA:A higher than one) would be associated with a lower rate of transplant-free survival.
To determine this, they reviewed UAB medical records for CF patients who had a lung transplant evaluation.
In total, the records of 78 CF patients with CT scan data, as part of their lung transplant work-up, were analyzed. Of these, 44 also had RHC data. The patients were 47% male, 97% white, and their mean age was 28 years.
Roughly half (38 of 78) of the patients showed signs of pulmonary artery enlargement — defined as a PA:A greater than one. These patients also exhibited higher pulmonary artery pressure (mPAP) and pulmonary vascular resistance, both symptoms of PH.
Pulmonary artery pressure refers to the pressure of blood pumping through the pulmonary artery. Pulmonary vascular resistance refers to the resistance that must be overcome to supply blood to the lungs. When this resistance is high, the heart must work harder.
Consistent with the researchers’ initial hypothesis, the transplant-free survival of patients with severe CF and PA enlargement was roughly seven months shorter than those without PA enlargement.
Pulmonary artery enlargement “was an independent predictor of PH,” and “was independently associated with increased hazards for death or transplant,” the researchers wrote.
Further investigation showed that shorter survival times correlated with an mPAP of 25 mm Hg or greater.
These results suggest that measuring the PA:A ratio is a viable way to test for PH among CF patients, and could be useful in making timely referrals for lung transplant evaluations.
The methods for making this measurement are already widely available, noninvasive, and likely to prove effective where other imaging techniques are less useful.
Nonetheless, the findings “should be confirmed in future, multi-center studies to further assess the utility of PA enlargement as a screening tool for PH in CF,” the researchers added.