Researchers ID strategies for treating chronic rhinosinusitis in CF
But more experiments are needed to determine treatments with greatest effect
Written by |
In laboratory experiments, a team of researchers in Belgium identified a few strategies that might help prevent bacteria from forming treatment-resistant clusters called biofilms that are believed to underlie chronic rhinosinusitis (CRS) — an inflammatory condition affecting the nasal passages and sinuses — in people with cystic fibrosis (CF).
Signs of CRS, in which there’s persistent inflammation in the sinus or nasal passages, can be observed in nearly all CF patients, with some experiencing symptoms such as a persistent runny or stuffy nose, sinus pain and pressure, and smell loss.
Among the beneficial strategies identified were baking soda salts, certain antibiotics, and phage therapy. Phage therapy uses bacterial viruses, or phages, instead of antibiotics, to treat bacterial infections.
Still, the scientists emphasized a need for more experiments to determine which treatments, alone or with others, have the greatest therapeutic effect.
“Further exploration … is necessary to optimize treatment combinations in clinical settings,” the team wrote.
Their study, “Evaluation of antibiofilm agents for treatment of cystic fibrosis-related chronic rhinosinusitis,” was published as a research note in the International Forum of Allergy & Rhinology.
Typical treatments for chronic rhinosinusitis often don’t work for CF patients
In individuals who don’t have CF, chronic rhinosinusitis is often treated with combinations of steroids, saline nasal rinses, and allergy medications. However, these standard methods don’t usually work as well in people with CF, in part because the underlying mechanism of the disease is different.
For people without CF, chronic rhinosinusitis is mainly characterized by inflammation driven by immune cells called eosinophils, which are commonly linked to allergic and inflammatory conditions. In CF, however, CRS is associated with inflammation caused by neutrophils, another type of immune cell that serves as a first responder to potentially harmful invaders, according to the researchers.
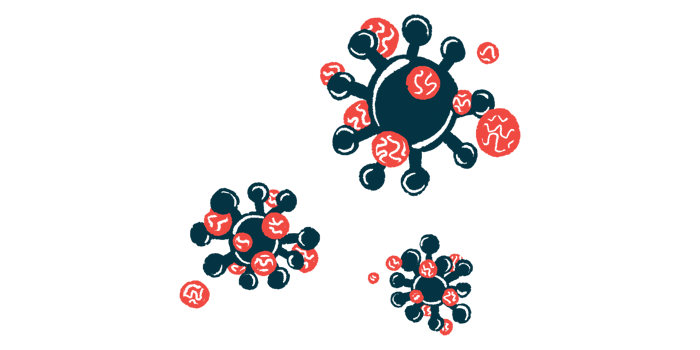
Moreover, the thick and sticky mucus that characterizes CF leads to the accumulation of harmful bacteria, such as Pseudomonas aeruginosa and Staphylococcus aureus, that contribute to sinus and nasal inflammation. These microbes join together to form biofilms, a type of protective cluster that helps them survive and makes them resistant to treatment.
The researchers believe that targeting these biofilms may be important for treating CF-related CRS. As such, they performed a series of lab experiments to investigate whether various treatments might be able to reduce CRS-related biofilms.
Results with certain treatments showed statistical significance
First, the researchers looked at whether the treatments could prevent biofilms from forming in the first place. A fluid designed to mimic CF sputum, or phlegm, was incubated with P. aeruginosa and S. aureus collected from the sinonasal passages of CF patients, along with various treatment combinations, and biofilm development was evaluated.
The team also investigated whether the same treatments could eradicate biofilms that had already formed. The sputum-like fluid was incubated with the bacteria overnight to allow them to form biofilms, and then later treated with the molecules.
Baking soda-enriched salts with or without added xylitol, a sugar alcohol found in some fruits and vegetables, reduced the numbers of both types of bacteria in both tests. That suggested some ability to both prevent and treat CF-related biofilm formation.
The scientists noted that xylitol has previously demonstrated an ability to inhibit CRS-related biofilms, especially when combined with other molecules.
High concentrations of the antibiotic levofloxacin reduced levels of already formed S. aureus biofilms, while the antibiotic ceftazidime significantly reduced P. aeruginosa biofilms.
While the results are statistically significant, their clinical relevance remains to be confirmed in trials.
Certain bacteriophages — bacteria-killing viruses that are gaining interest as possible treatments for antibiotic-resistant infections in CF — also had beneficial effects on the biofilms.
One phage called ISP significantly prevented S. aureus biofilm development, but couldn’t get rid of them after they’d already formed. Two types of phages, called PNM and 14-1, significantly reduced P. aeruginosa levels in both the prevention and treatment settings.
Combining some of the treatments led to even greater effects on biofilm formation. For example, combining low concentrations of levofloxacin with the phage ISP significantly lowered S. aureus levels relative to using just the antibiotics alone.
That could mean that certain combinations of antibiotics and phage therapies might be effective for targeting CRS biofilms in CF patients, according to the researchers.
Still, “while the results are statistically significant, their clinical relevance remains to be confirmed in trials,” the researchers wrote, adding that future studies should investigate “phage-antibiotic synergy.”