High rate of infections with SCVs found in CF patients in new review
Resistant-to-treatment infections may be due to use of antibiotic
Infections with Staphylococcus aureus small colony variants, known as SCVs, are highly prevalent in people with cystic fibrosis (CF) — and linked to the previous use of the broad-spectrum antibiotic trimethoprim sulfamethoxazole, a systematic literature review has found.
SCVs are slow-growing bacteria that are associated with higher rates of chronic infection in CF patients. These bacteria also tend to be highly resistant to antibiotics, contributing to the ineffectiveness of antibiotic treatment.
Furthermore, data also indicated that the presence of SCVs in CF patients was found to be associated with poorer lung function.
Researchers noted that “further investigation is necessary to determine the effect of infection by SCVs on the CF population.”
The study, “A systematic review of the clinical impact of small colony variants in patients with cystic fibrosis,” was published in the journal BMC Pulmonary Medicine.
Prior use of antibiotics found in patients with CF infections
CF is characterized by the accumulation of sticky and thick mucus in several organs, particularly the lungs and those of the gastrointestinal tract. In the lungs, mucus causes respiratory problems and provides a fertile ground for infectious bacteria.
Chronic bacterial infections in CF patients are associated with lung function decline and long-term use of antibiotics. In turn, antibiotic exposure is linked to the development of antibiotic-resistant bacteria and changes in SCVs.
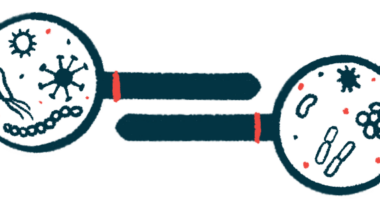
“To date, studies of SCVs have largely focused on two of the dominant [disease-causing bacteria] in people with CF, S. aureus and Pseudomonas aeruginosa (P. aeruginosa), with occasional reports of SCVs in other CF [disease-causing microbes],” the researchers wrote.
Now, researchers in Australia sought to investigate the prevalence of respiratory SCVs, as well as their clinical signs and risk factors. To that end, the team conducted a systematic literature review.
The review included 25 studies, most of them done in Europe and North America. Nearly two-thirds (64%) included both adults and children with CF; while 20% of the studies involved only children. Most of the studies — 21 in all — focused on the Gram-positive bacteria S. aureus. Others were focused on Gram-negative bacteria, mainly P. aeruginosa, as seen in three studies.
Gram-positive bacteria have a thick cell wall, whereas Gram-negative bacteria have thin cell walls. They release different toxins and cause different health issues.
Patients infected with SCVs of S. aureus were more likely to have previously used trimethoprim sulfamethoxazole, known as SXT, an antibiotic commonly used to treat respiratory infections in people with CF. The prevalence of SCVs in these patients was estimated to be at 19.3%.
Prior use of SXT also was more common in patients with SCVs than in those with non-SCVs (68.2% vs. 28.5%).
“This confirms the findings of other published studies that postulate that SCVs are an adaptive [manifestation] to antibiotic pressure and that SXT use in the treatment of S. aureus infections has been linked to the development of SCVs,” the researchers wrote.
SCVs linked to worse lung function in patients
The researchers also found that patients infected with SCVs of different types of bacteria had a forced expiratory volume in one-second percentage predicted (FEV1%) 16.8% lower than those infected with non-SCVs. FEV1% is a lung function parameter that measures the maximal amount of air a person can exhale in one second; its values are expressed in the form of a percentage of normal.
This is a “significant finding as morbidity in people with CF is often due to respiratory failure,” according to the team.
However, the scientists also noted that “lower lung function may not just be a result of SCV respiratory infection, as the lowered lung function observed may also be part of CF disease progression and co-morbidities.”
Bacteria were most commonly identified in respiratory sputum samples, followed by deep-throat respiratory swabs.
Gram-positive SCVs were described in most studies as being small, not tied to the destruction of red blood cells, greyish/non-pigmented, and slow-growing. In a limited number of studies, Gram-negative SCVs were described as being small and slow-growing.
The further study of SCVs and how they bring about … adverse outcomes will be necessary to better the treatment and management of CF in future.
“The assessment of SCVs is not currently routine practice in the work-up of CF respiratory samples in clinical microbiology laboratories,” the researchers wrote, noting that “long-term observational studies of the clinical outcomes of patients with SCVs are required to provide evidence of adverse impact to support outside use of a research setting.”
Considering the important role of bacterial infections in the poor health outcomes of CF patients, “the further study of SCVs and how they bring about these adverse outcomes will be necessary to better the treatment and management of CF in future,” the team wrote.