Synthetic Peptide Might Be Potential Treatment for Bacterial Infection Often Seen in CF Patients
Written by |
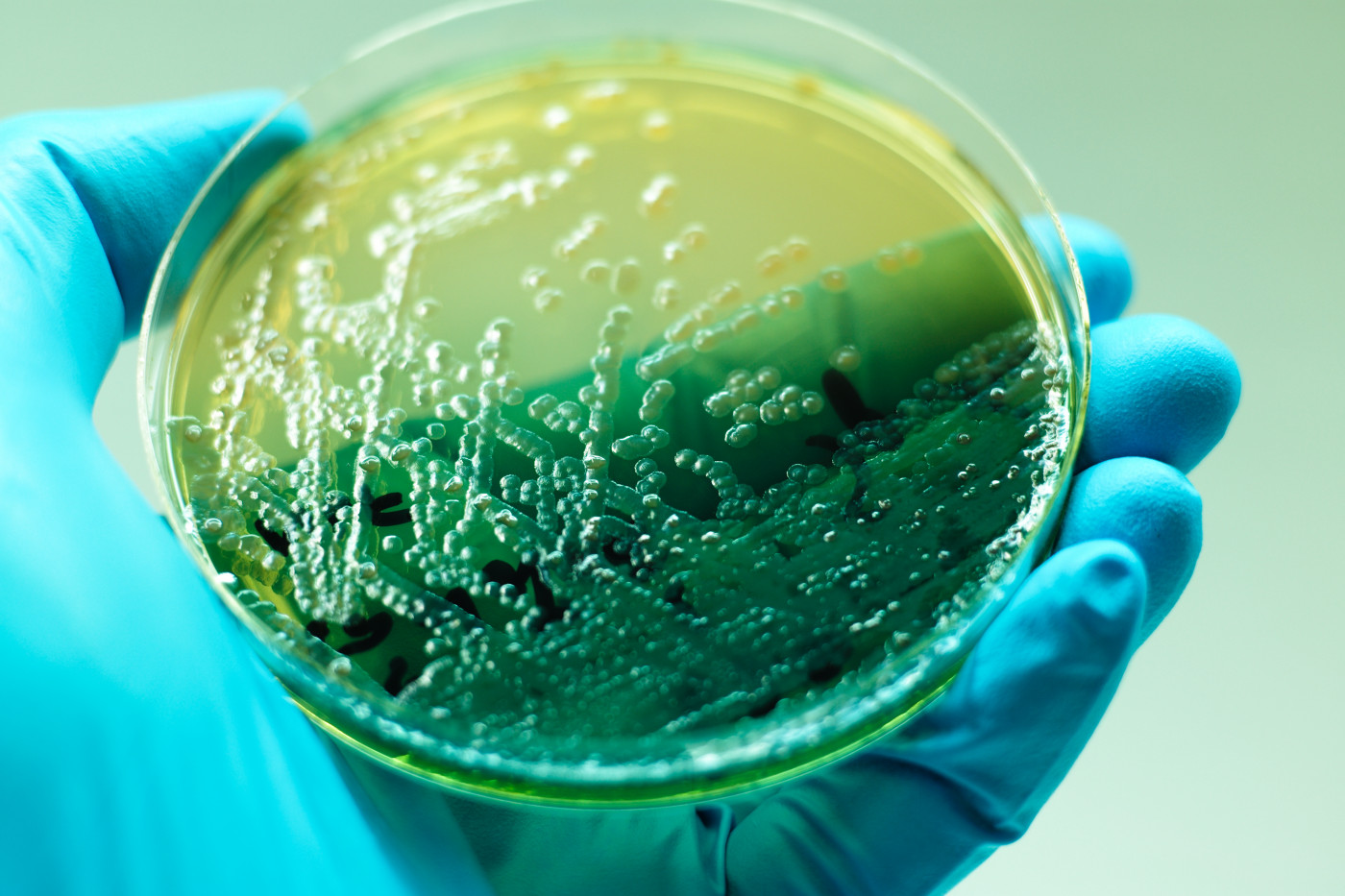
Pseudomonas aeruginosa is a bacteria that commonly infects cystic fibrosis patients. Now, researchers have designed a synthetic peptide that blocks the ability of these bacteria to cause disease.
This discovery might be crucial in fighting infectious diseases and preventing bacteria from becoming resistant to nearly all the antibiotic drug options available.
The paper titled “Targeting the alternative sigma factor RpoN to combat virulence in Pseudomonas aeruginosa,” was published in the journal Scientific Reports.
The work resulted from a collaboration between SUNY Upstate Medical University, SUNY College of Environmental Science and Forestry (both in Syracuse, New York) and the University of Ottawa (Ontario, Canada).
Pseudomonas aeruginosa bacteria are responsible for 10 percent of all hospital-acquired infections. They usually infect people whose immune systems have been compromised. Cystic fibrosis patients are also highly susceptible to infections by these bacteria.
In addition, Pseudomonas aeruginosa bacteria have a high intrinsic resistance to antibiotics, making it difficult to eradicate.
On the World Health Organization list of antibiotic-resistant pathogens for which new antibiotics are urgently needed and which should be targeted by researchers, Pseudomonas aeruginosa is in the top priority grouping, labeled as Critical.
With that in mind, scientists designed a lab-grown peptide (a small protein) that inhibited the production of the bacterial protein RpoN, which is known to be associated with several factors important to the bacteria’s virulence, such as motility and the ability to attach to a host. The peptide was called RpoN*.
RpoN* allowed researchers to regulate (turn off) the expression of certain genes in Pseudomonas aeruginosa that contribute to its virulence.
In Pseudomonas aeruginosa bacteria cultured in the lab, RpoN* was shown to significantly reduce the bacteria’s motility (ability to move spontaneously), secretion of protease (an enzyme that degrades proteins), and biofilm formation (a densely packed community of bacteria surrounded by a protective slimy, glue-like matrix). All are important parts of the infection process.
Then, the team explored the effects of RpoN* in a Caenorhabditis elegans–Pseudomonas aeruginosa infection model. Caenorhabditis elegans is a species of soil-dwelling roundworm (nematode) commonly used as a model organism in molecular genetics and developmental biology.
Researchers found that Caenorhabditis elegans survival was prolonged in the presence of RpoN*.
Taken together, the findings support RpoN* as an effective strategy for stopping Pseudomonas aeruginosa virulence. This approach could be key to the development of a possible treatment for cystic fibrosis patients and others susceptible to these bacteria.
“We’ve shown that there’s a mechanism through which we can slow the progress of bacteria in causing disease. And it could potentially inhibit the mechanism that creates resistance to antibiotics, which is obviously a huge concern,” Christopher Nomura, a professor of chemistry and vice president for research at SUNY College of Environmental Science and Forestry, said in a story on the college’s website.
“This synthetic peptide can be turned on at various times in the growth of bacteria. But right now, it still has to be done in a laboratory, where we can control its expression. There’s no way yet to deliver it, for instance, to a bacterial infection that might be making someone sick,” Nomura added.
Despite the fact that the peptide was only tested in one bacterial species, the findings likely apply to other types of bacteria, the team believes.
“With the spread of antibiotic resistance increasing, it is important to have as many tools as possible to address the issue. The development of this synthetic peptide will help with this process,” Nomura said.






