Asthma Medicine Xolair Successfully Treats Lung Allergy Due to Fungal Infection in 3 CF Patients, Case Report Shows
Xolair (omalizumab), a medicine used for allergic asthma and chronic hives, is effective for treating lung allergic reactions caused by fungi in patients with cystic fibrosis (CF), a case report suggests.
The study reports three cases of allergic bronchopulmonary aspergillosis in CF patients who were successfully treated with Xolair after conventional therapy with corticosteroids and antifungals failed.
The report, titled “Successful treatment with omalizumab of allergic bronchopulmonary aspergillosis in patients with cystic fibrosis: Case reports and literature review,” was published in The Journal of Allergy and Clinical Immunology: In Practice.
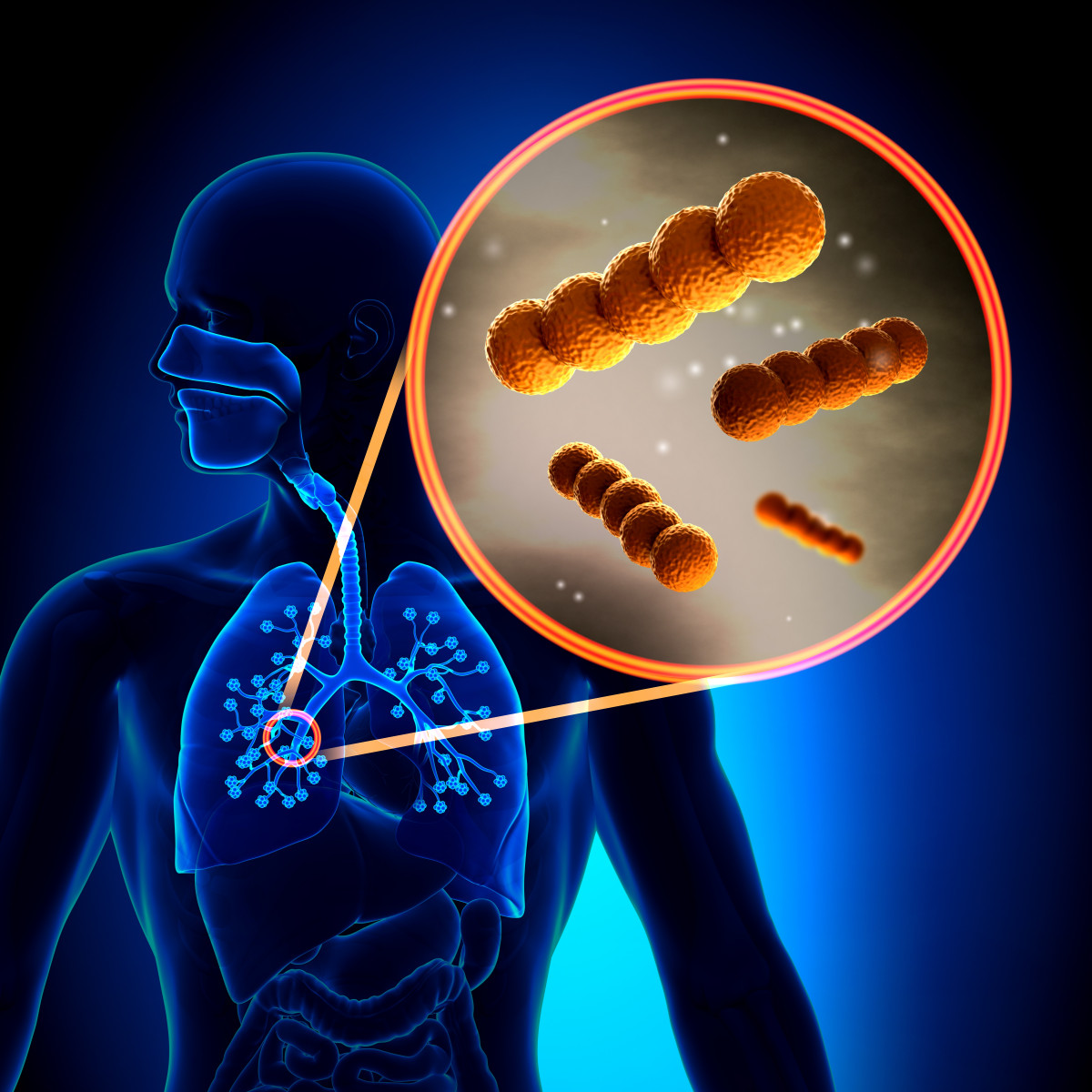
Allergic bronchopulmonary aspergillosis (ABPA), an allergic lung reaction caused by hypersensitivity to fungi of the genus Aspergillus, may affect 1% to 15% of patients with CF.
Xolair is a biologic agent (an antibody) approved for the treatment of uncontrolled allergic asthma and chronic spontaneous urticaria (chronic hives of unknown cause). It is given as an injection under the skin, and marketed by Genentech together with Novartis.
There is evidence that Xolair may also benefit patients with ABPA, given its ability to block immunoglobulin E (IgE), the major type of antibody involved in allergies.
The current study suggests that might be the case. The study describes the case of three male CF patients — ages 11, 17, and 28 — whose ABPA was successfully resolved after treatment with Xolair.
All three patients had breathing problems. The young boy was admitted to the hospital due to acute respiratory failure. The other two were having persistent dry cough in the previous months.
Discuss the latest research in the Cystic Fibrosis News Today forums!
All experienced progressive reduction in breathing capacity, seen by a decrease in predicted forced expiratory volume in one second (FEV1). In the young boy and the 17-year old male, predicted FEV1 reached 40%, whereas in the 28-year-old, it reached 50%.
Also, the airways of all three were infected by bacteria — namely Staphylococcus aureus, Pseudomonas aeruginosa, or both — and by the fungus Aspergillus fumigatus.
High-resolution computed tomography (HRCT) scans revealed widened airways, or bronchiectasis, in some lung lobes in all patients, as well as mucus plugging and air trapping in two of them.
ABPA was diagnosed on the basis of high blood IgE levels, positive skin prick test results for Aspergillus fungi, positive specific IgE for A. fumigatus, chest X-ray findings, and high blood counts of eosinophils (white blood cells that often get more abundant during allergic reactions).
Patients responded poorly to steroid and antifungal therapy, with none or only slight clinical improvements.
Therefore, treatment with Xolair was started, with dosages and dosing frequency based on the patient’s weight and their IgE values, as recommended for asthma treatment.
After eight weeks on Xolair, symptoms were eased, lung function was recovered — FEV1 increased to 68% in the 11-year-old, 93% in the 17-year-old, and 83% in the 28-year-old — and total IgE levels dropped to a normal range.
Attenuation of symptoms and improvement of breathing function were noted within two to four weeks of the first dose, and remained over a mean follow-up period of eight months.
“Our experience supports the safety and efficacy of this therapy,” the researchers wrote.
However, the team emphasized the lack of randomized clinical trials to confirm Xolair’s benefits assessing “both clinical and laboratory outcomes, including steroid requirement, ABPA exacerbations, and improvement in lung function,” they wrote.
Also, more data is needed to define the optimal dose and duration of treatment with Xolair “before this expensive therapy can be recommended as a routine treatment approach,” the researchers added.







