P. aeruginosa Thrives in CF Patients by Feeding Off Natural Bacteria in Lungs, Study Finds
Written by |
Interaction between bacteria naturally found in the lungs and disease-causing bacteria may make it harder to clear the pathogen from the body, a study reports. The finding is particularly important to people with cystic fibrosis (CF) because of their susceptibility to lung infections, and researchers hope their work will aid in developing better anti-bacterial treatments for these patients.
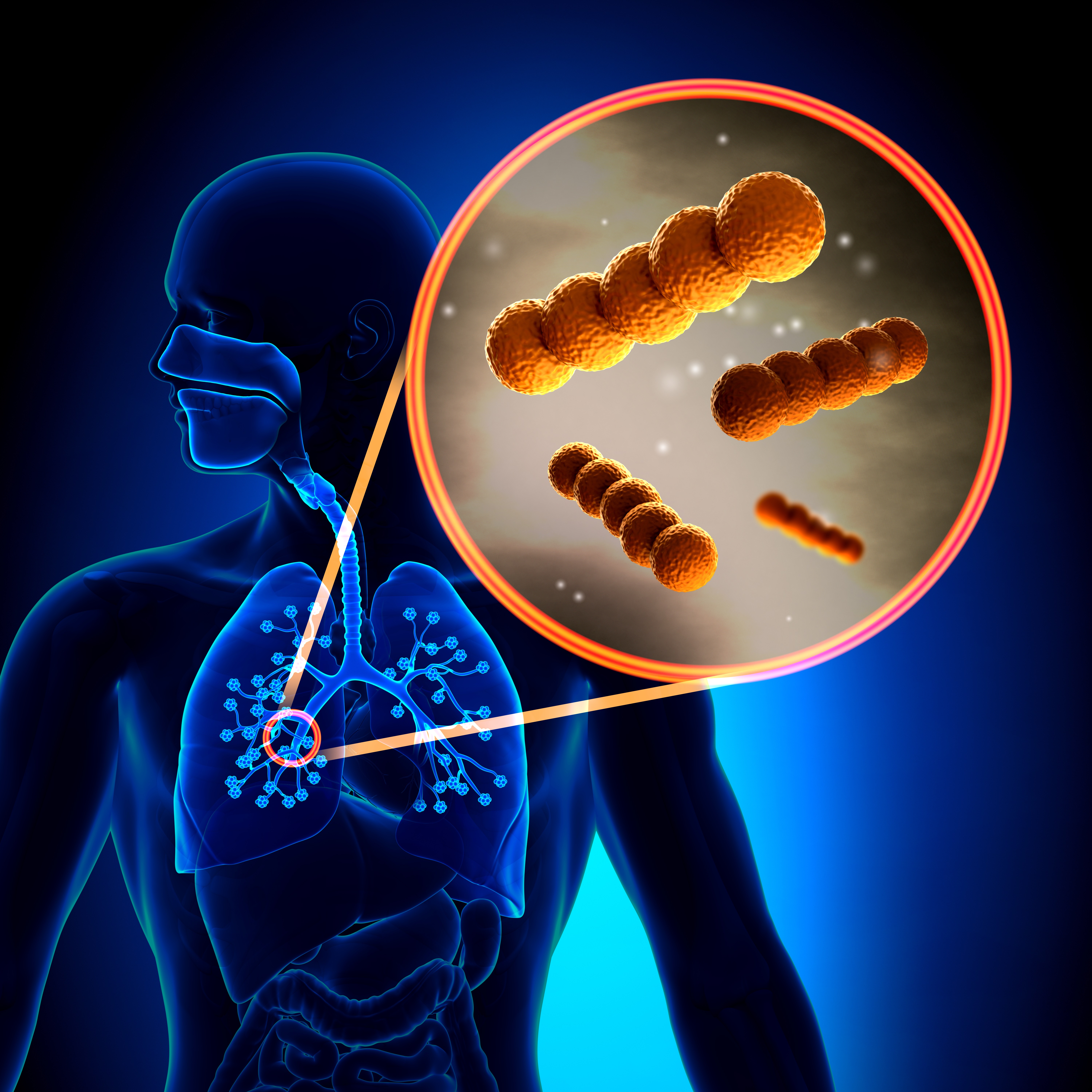
In the study, “The fermentation product 2,3-butanediol alters P. aeruginosa clearance, cytokine response and the lung microbiome,” published in The ISME Journal, researchers explored the relationship between a chemical (2,3-butanediol) produced by a bacteria that naturally lives in the lungs, and the common but harmful bacteria Pseudomonas aeruginosa, which is highly resistant in CF patients and the cause of lung inflammation.
The team infected one group of mice with P. aeruginosa, and a second group with P. aeruginosa plus the chemical produced by the resident bacteria.
Researchers saw that after three days, the second group of mice, those exposed to both the bacteria and 2,3-butanediol, had 100 times more bacteria in their lungs compared to the first group. This suggested that the chemical produced by common bacteria makes it harder for the body to clear P. aeruginosa infection from the lungs.
“Our findings show that we not only have to look at the bacteria itself, but we also have to look at the interaction of the natural bacteria in the lung,” Dr. Stefan Worgall, a distinguished professor of pediatric pulmonology and a professor of pediatrics and genetic medicine at Weill Cornell Medical College, said in a press release. The research was conducted at Weill.
According to the authors, it is important to better understand how P. aeruginosa infection settles in the lungs and how the bacteria interacts with other bacteria to find ways to effectively treat the infection.
People with CF take antibiotics regularly to help fight lung infections, but the efficacy of these treatments decline over time. The new findings might lead to better therapeutic strategies for CF patients, and for others who are highly susceptible to lung infections.






