Hyperbaric Oxygen Treatment May Make Antiobiotics More Effective Against P. aeruginosa Infections, Study Says
Exposing cystic fibrosis (CF) patients to high levels of oxygen through hyperbaric oxygen treatment may make Pseudomonas aeruginosa bacterial aggregates more sensitive to antibiotics like tobramycin and easier to eradicate from the lungs, a study in patient-derived bacterial cultures reports.
The study, “Hyperbaric oxygen treatment increases killing of aggregating Pseudomonas aeruginosa isolates from cystic fibrosis patients,” was published in the Journal of Cystic Fibrosis.
P. aeruginosa is the primary bacterium causing lung infections in CF patients. Tobramycin is an antibiotic often used to treat P. aeruginosa; however, chronic infections by this bacteria — which aggregates in the lungs and has biofilm-like properties — are often hard to eliminate.
Such treatment resistance by P. aeruginosa bacteria “may to some extend be explained by development of antibiotic tolerance in bacteria with reduced metabolic activity [inactive properties] due to a restricted supply of molecular oxygen,” the researchers wrote. In other words, bacteria slow their metabolism in an oxygen-deprived environment, lessening the effectiveness of antibiotics like tobramycin that are dependent on metabolic activity to work.
Of note, the mucus of CF airways is known to have very low oxygen levels (anoxic conditions).
Hyperbaric oxygen treatment, or HBOT, can be used both as a primary therapy or in combination with other therapies like antibiotics to enhance their efficacy. The procedure is performed in a hyperbaric oxygen chamber, and exposes patients to oxygen levels higher than atmospheric levels.
Interested in Cystic Fibrosis research? Sign up for our forums and join the conversation!
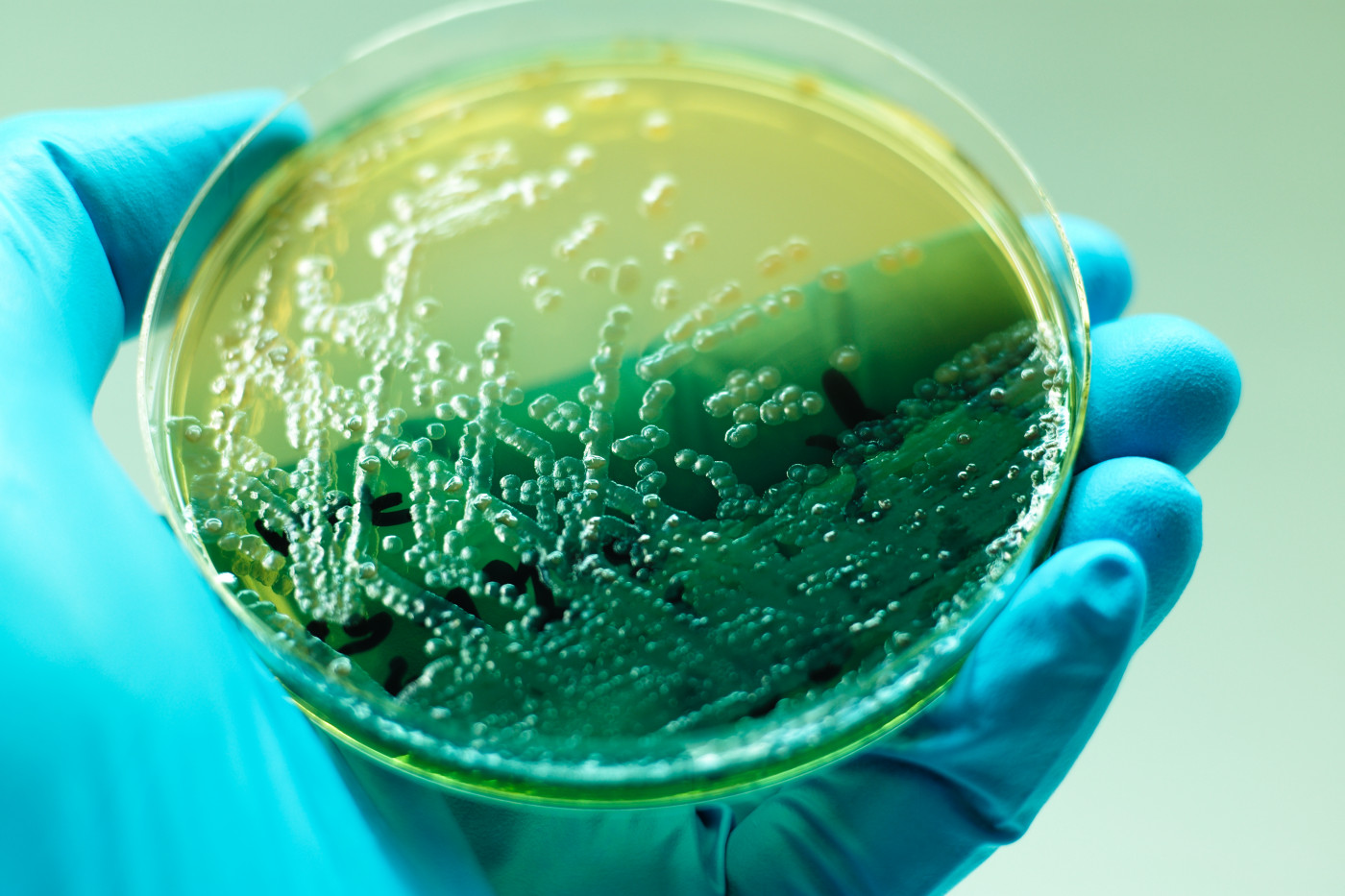
To test if increasing oxygen levels through HBOT could improve the effectiveness of tobramycin on P. aeruginosa, researchers exposed CF patient-derived bacterial cultures to the combination treatment in vitro (in a culture dish in the lab).
The team isolated 14 bacterial colonies (isolates) from the lungs and nasal cavities of three CF patients at different stages of P. aeruginosa colonization — including intermittently colonized, early chronic infection, and late chronic infection. The study included two separate reference P. aeruginosa strains (PAO1 and PDO300) as controls.
Then, researchers treated the bacteria cultures with different concentrations of tobramycin and incubated them in a hyperbaric oxygen chamber. An oxygen-free environment (anoxic) served as a control to the HBOT.
They found the tobramycin-induced killing of P. aeruginosa bacteria was significantly higher in the hyperbaric oxygen chamber than in the anoxic environment.
The reduction of bacterial colonies was also seen to be concentration-dependent, with higher tobramycin concentrations leading to more bacteria being killed.
Researchers next analyzed the effect of HBOT on bacterial colony formation by measuring changes in colony formation unit counts (an estimation of living bacteria in a sample) in the absence of tobramycin. They found a significantly higher number (1.11 log-fold) of these unit counts in bacteria exposed to HBOT, compared with unexposed bacteria.
To test if the increased colony formation resulted from HBOT-induced oxygenation, they followed the experiment by measuring oxygen consumption upon HBOT, using the PAO1 reference strain.
Results here showed that bacteria exposed to HBOT quickly consumed the oxygen, measured upon removal from the hyperbaric oxygen chamber. In contrast, bacteria treated with both HBOT and tobramycin consumed oxygen at a much lower rate, indicating that these bacteria were dying after tobramycin exposure in combination with HBOT.
Based on the results, the team suggested that HBOT increases tobramycin sensitivity in vitro by re-oxygenating and subsequently re-activating the bacteria’s metabolism and growth.
“Tobramycin is one of the common antibiotics used for P. aeruginosa eradication in CF patients, however, its effect relies on metabolically active bacteria,” the researchers wrote. “The current study provides evidence that manipulating the microenvironment around the [bacteria] aggregates can drive the otherwise inactive bacteria into active uptake of antibiotics.”
Although complications from HBOT use are rare, the research team recommended further study in animal models to confirm the safety and optimal administration of the combination therapy.
“Re-oxygenation may in the future be a clinical possibility as adjuvant to enhance killing by antibiotics in cystic fibrosis lung infections,” they concluded.