Nanoparticles in gene-editing therapy may correct CF defects
Optimizing nanoparticles, mucus-clearing treatment made therapy more efficient
Written by |
Researchers have developed nanoparticles that can deliver gene-editing therapeutics to correct genetic defects in the lungs of people with cystic fibrosis (CF).
The nanoparticles were optimized using cell-based models to penetrate the thick airway mucus seen in CF. Pretreating patients with the approved mucus-clearing agent Pulmozyme (dornase alfa) made the gene-editing therapy even more efficient, researchers said.
“Successful transmucosal delivery will offer great therapeutic opportunities not only for CF, but also other genetic lung diseases,” they wrote. The study, “Lung tissue-optimized gene editing in human cystic fibrosis models following topical application of lipid nanoparticles,” was published in the Journal of Controlled Release.
In CF, inherited mutations in the CFTR gene result in deficient or absent CFTR protein, leading to an abnormal buildup of thick, sticky mucus around various organs, including the airways.
Several approved therapies, such as CFTR modulators that correct CFTR protein defects, can improve lung function in CF. However, they don’t address the underlying genetic cause and aren’t effective in about 10% of patients who carry mutations that aren’t amenable to this type of therapy.
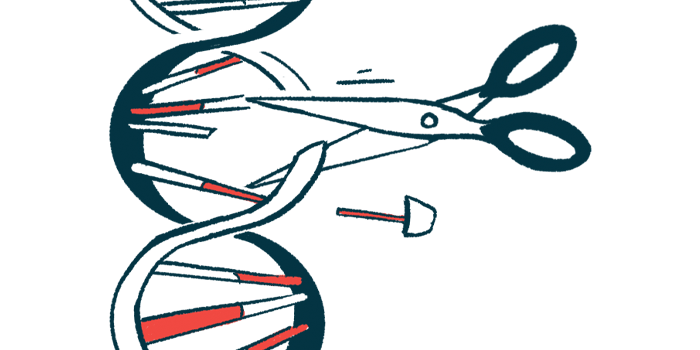
CRISPR-Cas9 is a gene-editing tool that may correct disease-causing mutations in previously untreatable conditions, including CF. It uses the Cas9 enzyme to cut DNA at a precise location, guided by a matching RNA sequence. However, delivering the genetic cargo to the lungs remains a significant challenge, due to thick mucus in the airways.
Lipid nanoparticles (LNPs) are tiny spheres composed of fat-like lipids that deliver drugs and genetic material to the body. Whether LNPs can overcome lung mucus to edit the airways’ target cells is unclear.
A gene-editing strategy for CF
Here, researchers in Germany and Canada developed a lung-tailored gene-editing strategy using LNPs and evaluated it in human cells and CF patient-derived models.
Initial experiments confirmed that commonly used LNP compositions led to low editing of a model gene, called HPRT, in human bronchial epithelial cells, which line the airways.
Researchers then optimized the LNPs to boost CRISPR-Cas9 gene-editing efficiency. Adding ionizable lipids, which are fat particles that can modulate their electric charge, depending on the environmental pH, significantly increased edit efficiency to 30%. Optimizing the guide RNA and the Cas9 messenger RNA, which carries the information stored in genes to make proteins, led to a 50% editing efficiency.
To mimic the lungs of a CF patient, the researchers developed a 3D airway model grown at an air-liquid interface using CF patient-derived bronchial epithelial cells, which harbor F508del, the most common CF-causing mutation. The model showed impaired CFTR protein function and thicker mucus, key features of CF.
In this model, the gene-editing efficacy rate dropped to 5%, which was “likely attributed to increased mucus secretion and viscosity, resulting in fewer LNPs reaching the epithelial cells,” wrote the researchers, who then pretreated the cells with Pulmozyme, following which, the gene-editing efficacy rose to as high as 12.7 %.
“While the significant drop of editing rates in 3D tissue models compared to the 2D monolayer cultures was expected, editing rates of [5%-10%] are potentially clinically relevant,” wrote the researchers, who also used the LNP system to repair a relatively common single CFTR mutation in CF patients called R1162X, which is untreatable with CFTR modulators.
Gene editing achieved a 12% efficiency rate in cells lining the nasal cavity. “This study presents a systematic approach to optimize gene-editing efficacies in 2D and 3D human lung models, yielding clinically relevant … editing rates in 3D CF disease models following topical application.”