In-school treatment may improve health outcomes for CF children
Use of airway clearance therapy at school may increase adherence

In-school use of airway clearance therapy (ACT) improved a number of health outcomes for children with cystic fibrosis (CF) who had poor adherence to ACT at home, according to a new study.
In the year after starting ACT at school, the children experienced significant reductions in the number of pulmonary exacerbations — acute worsening of lung symptoms — that required antibiotics compared with the year before. The children also had fewer days overall on antibiotics, and fewer visits to the CF care center.
The study, conducted in New York, reviewed the results of a collaboration between a CF care center and local schools that sought to improve ACT adherence among pediatric patients.
“This relationship resulted in multiple improved CF health outcomes,” the researchers wrote, noting that “continued focus needs to be placed on identifying individual barriers to adherence early in disease management.”
The study, “Airway clearance therapy in the school environment: Retrospective analysis of a cohort of pediatric patients with cystic fibrosis,” was published in the Journal of Cystic Fibrosis.
Better outcomes found with airway clearance therapy at school
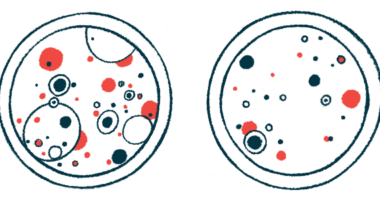
Airway clearance therapy, dubbed ACT, aims to loosen the thick, sticky mucus that continually builds up in the lungs of CF patients. Such treatments enable the mucus to be more easily cleared by coughing.
Approaches include high frequency chest wall oscillation (HFCWO) and positive expiratory pressure (PEP), which, in different ways, put pressure on the airway walls to force the mucus away from them.
These approaches are generally intended to be used at home daily to continuously keep the lungs clear — and their success relies on appropriate adherence to the ACT regimen.
However, adherence reportedly is low for pediatric CF patients, with reports suggesting that compliance among children may be below 50%.
In turn, poor adherence is linked to lung function declines, pulmonary exacerbations, and an increased hospitalization risk.
“Adherence to therapy is therefore essential to prevent worsening of CF in the pediatric population,” the researchers wrote.
Because children spend a lot of time at school, the implementation of ACT in the school setting may be one way to boost ACT adherence. The Cystic Fibrosis Center of Western New York began a collaboration with local schools to work toward that goal.
In the study, researchers retrospectively reviewed the impact of this school program on lung function and healthcare utilization in a group of 14 pediatric CF patients. The children had a mean age of 13.7.
These six girls and eight boys, who were previously identified as having inadequate ACT adherence at home, received treatments at school for at least one year. A school employee was trained by a respiratory therapist to administer airway clearance therapy to the children.
A group of 36 children with CF who had self-reported adequate use of ACT at home also were included in the analysis as a control group.
Significantly more children in the control group were Caucasian (100%) than in the at-school ACT group (71.4%). Most children in both groups — 13 in the school group and 33 in the control group — were using HFCWO as the type of ACT.
Trying to increase adherence
In the year before starting ACT at school, children in the school group had significantly more pulmonary exacerbations requiring antibiotics, more total days of antibiotics usage, and more days of into-the-vein (intravenous) antibiotics compared with the control group.
These children also visited the CF care center more often and had a greater number of days of hospitalization.
After starting ACT at school, the children experienced significant reductions in the number of pulmonary exacerbations requiring antibiotics and fewer days of antibiotics treatment. They also needed fewer visits to the CF care center, reaching levels comparable to the control group after a year.
This partnership allowed clinicians to utilize a built-in facet of a child’s life, mandatory education, as a means to ensure patients with CF received ACT.
Lung function testing was conducted among children who were old enough. It showed lung function was worse in the school group at the study’s start compared with controls, and was not significantly changed after a year of school ACT.
Overall, initiating ACT in school seemed to improve health outcomes for CF children who previously had low adherence to ACT at home.
Given the racial disparities in the two groups of children, “it is unclear to what extent race played a role in differences across outcome variables between our groups,” the researchers noted.
Still, the CF Foundation‘s efforts with local schools reflects a commitment to “identify barriers to treatment and develop solutions in order to sustain daily care,” they wrote.
Moreover, “this partnership allowed clinicians to utilize a built-in facet of a child’s life, mandatory education, as a means to ensure patients with CF received ACT.”
“Ideally, a prospective study would replicate these results,” the team added.
Among the study’s limitations were its small sample size and a lack of random assignment that may have allowed potential selection bias among participants.
The team noted that future studies also will need to evaluate the success of such programs in geographical areas where a CF center isn’t nearby, and thus, clinicians aren’t able to work as closely with school systems.